
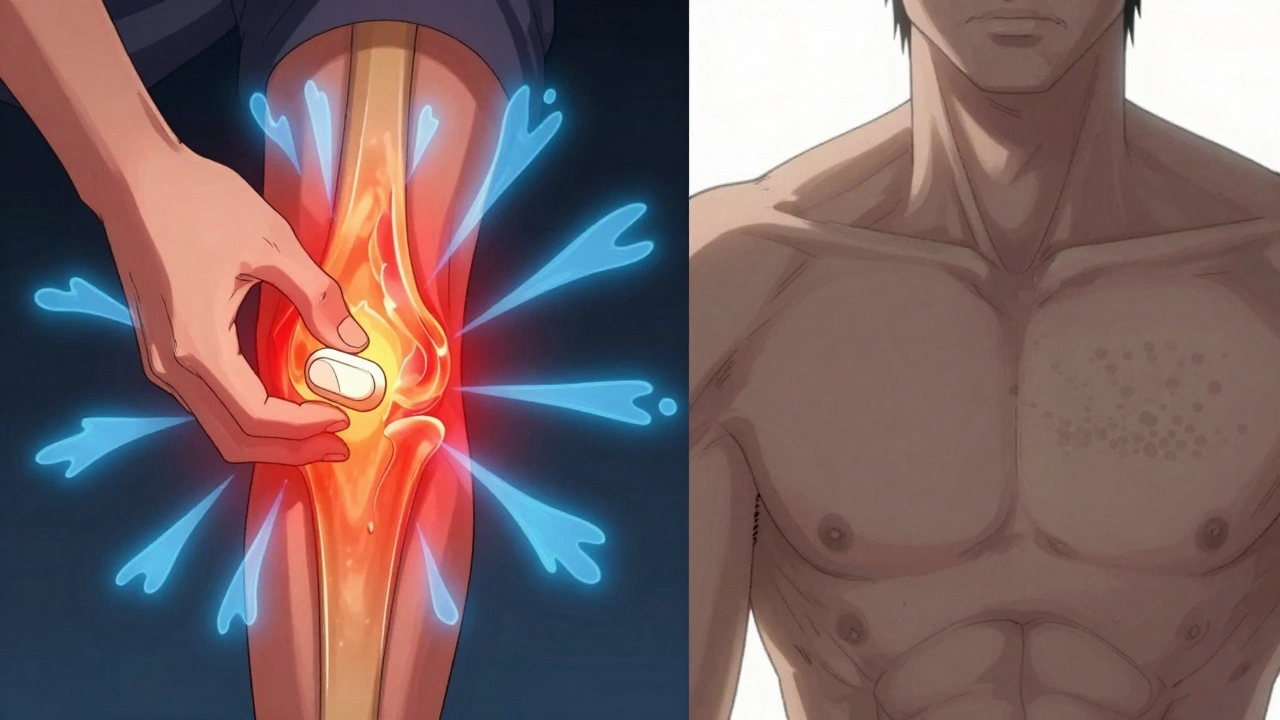
When you twist your ankle, slam your finger in the door, or get a bad case of arthritis, the pain you feel isn’t random. It’s your body’s alarm system kicking in - and that’s nociceptive pain. It’s the most common type of pain you’ll ever experience. Around 85% of acute pain cases, from sprains to post-surgery soreness, fall into this category. Unlike nerve damage pain or mysterious chronic pain, nociceptive pain has a clear source: damaged tissue. And knowing that changes everything about how you treat it.
What Exactly Is Nociceptive Pain?
Nociceptive pain happens when your body’s pain sensors - called nociceptors - get triggered by real or potential harm. These sensors live in your skin, muscles, joints, bones, and even internal organs. They don’t care about your mood or stress level. They react to physical damage: heat, pressure, cuts, swelling, or chemical changes from inflammation.
There are three main types:
- Superficial somatic: Sharp, pinpoint pain from cuts or burns. Think stubbing your toe - it’s fast and local.
- Deep somatic: Dull, aching, hard-to-pinpoint pain from muscles, tendons, or bones. A pulled hamstring or broken rib fits here.
- Visceral: Deep, crampy, or pressure-like pain from organs. Gallstones or a stomach ulcer cause this kind. It often feels vague and spreads out.
The key? This pain follows the healing timeline. If the tissue heals, the pain fades. That’s why treating the cause - not just hiding the signal - matters so much.
Why NSAIDs Work Better for Most Injuries
NSAIDs - like ibuprofen, naproxen, and aspirin - don’t just numb pain. They attack the root. They block enzymes called COX-1 and COX-2, which your body uses to make prostaglandins. These are the chemicals that cause swelling, redness, and heat around an injury. Less swelling? Less pressure on nerves. Less pain.
Here’s what the data says:
- In a 2023 Cochrane Review of over 7,800 patients, ibuprofen 400mg gave 50% pain relief to 49% of people with acute sprains or strains. Placebo? Only 32%.
- For osteoarthritis, the American College of Rheumatology recommends NSAIDs as first-line - not acetaminophen. Why? Because inflammation drives the pain.
- On Reddit’s pain community, 68% of users preferred NSAIDs for injury-related pain. One physical therapist wrote: “I recommend 600mg ibuprofen three times a day for ankle sprains. It cuts recovery time by 2-3 days.”
NSAIDs shine when there’s visible swelling, warmth, or redness. That’s your body’s inflammatory response. NSAIDs quiet that down. No inflammation? Less pain.
Where Acetaminophen Falls Short - and When It Still Helps
Acetaminophen (paracetamol) is everywhere. It’s in Tylenol, Excedrin, and countless cold medicines. But here’s the truth: it doesn’t reduce inflammation at all. Not even a little.
Its mechanism is still partly a mystery. It might act on brain receptors (COX-3), affect serotonin, or modulate pain signals in the spinal cord. But it doesn’t touch the swollen knee or inflamed tendon. That’s why it’s weak for injuries.
- A 2022 JAMA meta-analysis found acetaminophen helped only 39% of people with acute low back pain. Ibuprofen? 48%.
- The American Headache Society still calls acetaminophen first-line for tension headaches - because there’s no major inflammation involved.
- On Drugs.com, 74% of users rated acetaminophen highly for mild headaches. Why? “No stomach upset,” said 42% of positive reviewers.
So acetaminophen isn’t useless. It’s just misused. Use it for mild, non-inflammatory pain: a headache, a toothache without swelling, or a minor muscle ache after a workout. Don’t use it for a sprained ankle or inflamed joint.
The Safety Trade-Offs You Can’t Ignore
Both drugs have risks - but they’re very different.
NSAIDs:
- Stomach ulcers: 1-2% annual risk with regular use. Can lead to bleeding.
- Heart risks: High-dose diclofenac doubles heart attack risk (The Lancet, 2017).
- Kidney strain: Especially in older adults or those dehydrated.
Acetaminophen:
- Liver damage: The max safe dose is 4,000mg/day - but many people exceed it by combining cold meds, painkillers, and sleep aids.
- Overdose can be fatal at just 150-200mg/kg. That’s 10-14 standard tablets for an adult.
- 22% of negative reviews mention “liver scare” - people panic after taking too much.
Bottom line: NSAIDs hurt your stomach and heart. Acetaminophen hurts your liver. Neither is “safer” - they’re just different dangers.
When to Use Which - A Simple Rule
Here’s how to pick, fast:
- Is there swelling, redness, or warmth? → Use NSAID (ibuprofen 400-600mg every 6-8 hours).
- Is it a dull, constant ache with no inflammation? → Use acetaminophen (650-1,000mg every 6 hours).
- Is it a headache with no sinus pressure or swelling? → Acetaminophen is fine.
- Is it a sprain, strain, or post-surgery pain? → NSAID. Always.
And if you’re unsure? Start with acetaminophen. If pain doesn’t improve in 24-48 hours, switch to NSAID - but only if there’s swelling.

What About Combining Them?
Many people take both together - and it works. A 2022 Mayo Clinic survey found 61% of chronic pain patients used combo therapy. They reported 32% better pain control than either drug alone.
That’s smart for mixed pain: say, osteoarthritis with occasional flare-ups. Take acetaminophen daily for baseline pain, then add ibuprofen only on bad days.
But don’t overdo it. Stick to these max doses:
- NSAID: No more than 1,200mg ibuprofen per day without a doctor’s note.
- Acetaminophen: Never exceed 3,000mg/day if you drink alcohol, have liver disease, or are over 65.
What’s New in Pain Relief?
There’s progress on the horizon.
- Topical NSAIDs: Diclofenac gel. You apply it right on the knee or elbow. Only 30% gets into your bloodstream - way fewer side effects.
- Combination pills: The FDA approved Qdolo (tramadol + acetaminophen) in 2022 for moderate-to-severe pain. Still not for inflammation, but better for stubborn cases.
- Future drugs: Eli Lilly is testing LOXO-435, a new pill targeting specific pain receptors in internal organs. Early trials show 40% pain reduction in IBS patients.
Meanwhile, traditional NSAIDs still dominate the market - $13.7 billion in 2023. Acetaminophen? $5.8 billion. But NSAIDs are growing faster because they actually treat the problem - not just the symptom.
Final Takeaway: Treat the Injury, Not Just the Signal
Nociceptive pain isn’t something to silence. It’s a message. And if you ignore the message, you might miss the healing.
NSAIDs are the right tool when tissue is damaged and inflamed. They reduce swelling, speed recovery, and lower the chance of chronic pain developing.
Acetaminophen is a gentle option for mild, non-inflammatory pain. It’s kinder to your stomach, but it doesn’t fix anything - it just makes the noise quieter.
Choose based on what’s happening in your body - not what’s on sale at the pharmacy. If your knee is swollen, reach for ibuprofen. If you have a tension headache, acetaminophen is fine. And if you’re unsure? Ask your pharmacist. They know the difference.
Don’t just take painkillers. Understand why you’re taking them.
Is acetaminophen better than NSAIDs for back pain?
No - not if the back pain comes from inflammation, like a muscle strain or arthritis flare-up. Studies show ibuprofen works better. Acetaminophen only helps mild, non-inflammatory back pain. For most people with acute low back pain, NSAIDs provide significantly better relief.
Can I take ibuprofen and acetaminophen together?
Yes, and many people do. Combining them can give better pain control than either alone - especially for mixed pain types. Just don’t exceed the daily max: 4,000mg of acetaminophen and 1,200mg of ibuprofen. Avoid if you have liver or kidney issues.
Why do doctors recommend NSAIDs for arthritis but not acetaminophen?
Because arthritis involves joint inflammation. NSAIDs block the chemicals that cause swelling and pain. Acetaminophen doesn’t touch inflammation - so it’s ineffective for the root cause. The American College of Rheumatology downgraded acetaminophen for arthritis in 2023 because studies showed it barely works.
Is it safe to take NSAIDs every day for chronic pain?
Long-term daily use increases risks: stomach ulcers, kidney damage, and heart problems. For chronic pain, doctors prefer the lowest effective dose for the shortest time. Topical NSAIDs or non-drug therapies (like physical therapy) are safer long-term options. Always talk to your doctor before daily NSAID use.
What’s the safest painkiller for older adults?
For mild pain without inflammation, acetaminophen is usually safest - but only if liver function is normal and doses are kept under 3,000mg/day. For joint pain with swelling, topical NSAIDs (like diclofenac gel) are preferred over oral ones to avoid stomach and kidney risks. Avoid NSAIDs entirely if they have heart disease or kidney issues.
Does acetaminophen help with swelling?
No. Acetaminophen does not reduce swelling or inflammation. It only reduces pain signals in the brain. If your ankle is swollen after a sprain, acetaminophen will not make the swelling go down - ibuprofen will.

nikki yamashita
December 13, 2025 AT 01:21NSAIDs for sprains, acetaminophen for headaches. Simple. Done.
Nathan Fatal
December 13, 2025 AT 18:01This is one of the clearest breakdowns of nociceptive pain I’ve seen in years. Most people treat pain like a software bug to be patched, not a biological signal to be understood. The body isn’t broken-it’s communicating. NSAIDs don’t just mask pain; they reduce the inflammatory cascade that delays healing. Acetaminophen? It’s like turning off the alarm clock without fixing the fire. You’ll sleep longer, but the house is still burning.
And yes, the Cochrane data is solid. I’ve seen patients with ankle sprains go from 7/10 pain to 2/10 in 48 hours with 600mg ibuprofen every 8 hours. Placebo? Barely a blip. The real win? Faster return to mobility. That’s not just pain relief-that’s functional recovery.
Robert Webb
December 14, 2025 AT 09:22I appreciate how this post avoids the oversimplification that ‘all pain is the same’-which is unfortunately rampant in both medical education and consumer health culture. Pain is a multidimensional experience, and nociceptive pain is the most straightforward kind because it has a clear, identifiable origin. That’s why it’s also the most treatable.
What’s interesting is how often people confuse nociceptive pain with neuropathic or nociplastic pain-especially when they’ve been told ‘it’s all in your head’ after acetaminophen failed them. The truth is, if there’s swelling, heat, redness, or tenderness to touch, you’re dealing with inflammation-and that’s where NSAIDs belong. Acetaminophen might make you feel slightly better, but it won’t change the underlying biology. It’s like using a bandage on a leaky pipe.
Also, the point about combination therapy is crucial. Many chronic pain patients aren’t being told they can layer treatments safely. The 32% improvement with combo use isn’t magic-it’s pharmacology. Different mechanisms, additive effects. And yes, dosing matters. Don’t stack 1000mg of acetaminophen with 800mg of ibuprofen every 4 hours. That’s how you end up in the ER. But 650mg + 400mg every 6 hours? That’s smart, evidence-based, and sustainable.
Topical NSAIDs are underrated. I’ve had patients with knee osteoarthritis who couldn’t tolerate oral meds due to GI issues. Diclofenac gel? Game-changer. Local effect, systemic exposure minimal. And for older adults? That’s the new gold standard. No more guessing whether the liver or the stomach will give out first.
Finally, the future drugs like LOXO-435? Fascinating. Targeting visceral pain receptors specifically could revolutionize IBS and chronic abdominal pain. Right now, we’re stuck with opioids or nothing. If this works, we might finally have a non-addictive, non-inflammatory option for organ-based pain. I’m watching the trials closely.
Adam Everitt
December 15, 2025 AT 19:00nsaids r good for swelling but like… dont they mess up your gut? i mean i took ibuprofen for a week after i twisted my ankle and felt like my stomach was a hole. also, why do people say ‘acetaminophen doesnt work’? i took it for my back and it was fine? maybe im just lucky? or maybe my pain isnt ‘real’ enough for you guys?
also, i heard somewhere that tylenol causes liver damage if you drink? is that true? or is that just fearmongering? i like my whiskey and my painkillers. why cant i have both? 😕
wendy b
December 17, 2025 AT 09:22Let me correct the misinformation here. The claim that NSAIDs ‘speed recovery’ is not supported by robust longitudinal studies. The Cochrane review you cite measures pain relief-not healing time. There is zero evidence that reducing inflammation accelerates tissue repair; in fact, inflammation is a necessary phase of healing. By suppressing it, you may be delaying collagen deposition, fibroblast activity, and angiogenesis.
Furthermore, the American College of Rheumatology’s recommendation is based on short-term symptom control, not disease modification. Arthritis is not ‘inflammation’-it’s degeneration. NSAIDs do nothing to halt cartilage loss. They merely mask discomfort, which may even encourage overuse and further joint damage.
And acetaminophen? It’s not ‘ineffective.’ It’s underutilized because it lacks the flashy anti-inflammatory branding. Its mechanism is complex, yes-but that doesn’t make it inferior. In fact, for elderly patients with comorbidities, it’s the only viable option. Your binary ‘swelling or no swelling’ rule is dangerously reductive. Pain is subjective. Your algorithm ignores individual physiology, genetics, and psychosocial factors.
This post reads like a pharmaceutical marketing brochure. It’s not science. It’s simplification with authority.
Rob Purvis
December 18, 2025 AT 08:27Great breakdown-thank you for the clarity. I just want to add one thing: the 2023 Cochrane review on ibuprofen for sprains? The number of patients who achieved 50% pain relief was 49%, but the number who reported ‘clinically meaningful improvement’-meaning they could walk without crutches or sleep through the night-was 67%. That’s the real win.
Also, for anyone thinking ‘I’ll just take acetaminophen because it’s gentler’-remember: the liver doesn’t feel pain until it’s too late. 4,000mg is the max, but most people don’t realize that NyQuil, Excedrin, and cold meds all contain acetaminophen. One night of ‘just one more’ for a headache? You’ve hit 3,000mg before breakfast. Add a glass of wine? You’re in danger zone. I’ve seen two patients in my clinic with acute liver failure from ‘accidental’ overdose. Both thought they were being careful.
And yes, topical NSAIDs are underused. I prescribe diclofenac gel to every older patient with knee OA. No GI risk, no kidney strain. Just rub it on, wait 15 minutes, and go about your day. It’s like a tiny, targeted NSAID missile. Why take a sledgehammer when you have a scalpel?
Finally, the combo therapy point? Absolutely. I tell patients: ‘Use acetaminophen like your daily multivitamin-steady, low dose. Use NSAIDs like your emergency flare-up kit-only when the joint is hot, swollen, and screaming.’ That’s not just smart-it’s sustainable.
Laura Weemering
December 19, 2025 AT 18:16Okay, but… who funds these studies? Who benefits from pushing NSAIDs? Big Pharma? The same companies that made opioids? The same ones that downplayed acetaminophen’s liver risks for decades? And now they’re telling us NSAIDs are ‘better’ because they ‘treat the cause’? What cause? The cause is capitalism. They want you to keep buying pills. They don’t want you to rest. They don’t want you to ice it. They don’t want you to see a PT. They want you to pop a pill and keep working.
And the ‘68% prefer NSAIDs’ statistic? That’s from Reddit. Not a journal. Not a double-blind trial. Reddit. Where people think ‘I felt better’ is science.
What about the 2021 study in The BMJ showing that NSAID use for acute low back pain increased the risk of chronic pain by 30%? Because suppressing inflammation too early disrupts the natural healing cascade?
I’m not saying acetaminophen is perfect. But I’m saying: don’t trust the narrative. Don’t trust the ‘simple rule.’ Don’t trust the ‘data.’ Trust your body. And if your body says ‘rest,’ then rest. Not ibuprofen. Rest.
Audrey Crothers
December 19, 2025 AT 18:49THIS. THIS RIGHT HERE. 😭 I twisted my ankle last month and took Tylenol for 3 days-nothing. Then I tried ibuprofen? I could walk without limping by day 2. My ankle didn’t look like a balloon anymore. I cried. Not from pain-from relief.
Also, my grandma takes acetaminophen every day for ‘aches’ and her liver enzymes are through the roof. She didn’t even know her cold medicine had it too. Please, everyone-read the labels. It’s not hard.
Topical NSAIDs? YES. I use the gel on my knees and I don’t even feel it go on. No stomach issues. No weird side effects. Just quiet pain. I’m telling all my friends.
Thank you for writing this. It saved me from making dumb choices. 💪
Stacy Foster
December 21, 2025 AT 18:38NSAIDs are a gateway drug to heart attacks. Acetaminophen is a silent killer. Both are controlled by the FDA, which is owned by the same corporations that make them. You think this is about pain? It’s about control. They want you dependent. They want you believing you need pills to function. The truth? Your body heals faster without drugs. Ice. Rest. Elevation. That’s it. No pills. No ‘science.’ Just biology.
And the ‘61% use combo therapy’? That’s not a win-that’s a red flag. You’re not healing. You’re chemically masking. They don’t want you to heal. They want you to keep buying.
They’re lying to you. Always.
Reshma Sinha
December 23, 2025 AT 16:39As a physiotherapist in Mumbai, I see this daily. Patients come in with knee pain, take ibuprofen for a week, then wonder why it’s still swollen. I explain: ‘Painkiller ≠ healer.’ We need movement, not medication. NSAIDs help with inflammation, yes-but if you don’t restore mobility, you’re just delaying the real work.
And acetaminophen? Used properly, it’s fine for mild pain. But in India, people buy it over the counter without knowing doses. I’ve seen 10 tablets a day for weeks. Liver failure. Preventable.
Topical NSAIDs? Not widely available here. But ice packs? Yes. Compression? Yes. Rest? Rarely. We need education, not just prescriptions.
Also-combining drugs? Only under supervision. One patient took Tylenol + diclofenac + a cold syrup. Triple dose. ICU. Don’t be that person.
Lawrence Armstrong
December 24, 2025 AT 08:24Just want to say: this is the kind of post that makes Reddit worth it. 🙌
Topical NSAIDs are a game-changer. I’ve been using diclofenac gel on my shoulder for months. No stomach issues. No kidney stress. Just relief. I didn’t even know it existed until last year.
And yes-combining acetaminophen and ibuprofen? Works wonders for my chronic lower back. I take 650mg acetaminophen in the morning and 400mg ibuprofen at night. No side effects. Pain down from 8 to 3. I’m not addicted. I’m optimized.
Thanks for the data. This is the info we need more of.
Donna Anderson
December 26, 2025 AT 03:12i just took tylenol for my headache and now i feel like a genius 😎
also i think nsaids are for people who like to be dramatic about pain
my ankle was swollen but i just drank water and it got better. no pills needed. 🌿
Levi Cooper
December 27, 2025 AT 18:59Wow. So you’re telling me that American doctors are right about pain? That the FDA knows what’s best? That science is reliable? What’s next? You’ll tell me vaccines work? That climate change is real?
Let me guess-you also believe in ‘evidence-based medicine’ and ‘peer-reviewed studies.’ How quaint. In my country, we treat pain with prayer and turmeric. No pills. No corporate lies.
Why do you trust the system that got you addicted to opioids? Why do you trust the same people who lied about cigarettes?
Wake up.
NSAIDs are poison. Acetaminophen is poison. The system is poison.
Just say no.
Nathan Fatal
December 28, 2025 AT 04:06Wendy, your critique sounds sophisticated-but it’s built on a strawman. Nowhere did I say NSAIDs ‘accelerate healing’ as a biological certainty. I said they reduce inflammation that delays mobility and increases risk of chronic pain. There’s a difference.
Yes, inflammation is part of healing-but uncontrolled, prolonged inflammation causes collateral damage: cartilage breakdown, fibrosis, nerve sensitization. NSAIDs don’t shut down inflammation entirely-they bring it back to physiological levels.
And the ‘Reddit data’? I cited it as anecdotal support, not primary evidence. The Cochrane and JAMA studies are the backbone. You’re rejecting the data because you distrust the messenger? That’s not skepticism-it’s denial.
Also, ‘rest’ is vital. But rest + NSAID is better than rest alone. One doesn’t cancel the other.
And yes-I’ve seen patients who didn’t take anything and ended up with chronic pain because they waited too long. Pain isn’t just a signal. Left unchecked, it rewires the nervous system. That’s not a conspiracy. That’s neuroplasticity.