
Every year, millions of people reach for ibuprofen or naproxen to ease a headache, back pain, or menstrual cramps. These are the two most common over-the-counter NSAIDs - simple, fast-acting, and seemingly harmless. But what if the bottle you’re holding could quietly raise your risk of a heart attack, stomach bleed, or kidney damage - even if you take it just once a week? Most people don’t know the real risks. And that’s dangerous.
What You’re Actually Taking
When you buy Advil or Motrin, you’re getting ibuprofen - usually 200 mg per tablet. Aleve? That’s naproxen sodium, 220 mg per tablet. Both are NSAIDs, which means they block enzymes that cause pain and swelling. Sounds good, right? But here’s the catch: they don’t just block the bad enzymes. They also block the good ones that protect your stomach lining and help your kidneys function properly.
The difference between ibuprofen and naproxen isn’t just brand names. Ibuprofen wears off in about 2 hours. That’s why you’re told to take it every 4 to 6 hours. Naproxen lasts 12 to 17 hours. That’s why you only need it every 8 to 12 hours. But longer-lasting doesn’t mean safer. In fact, naproxen sticks around long enough to build up in your system, which can increase the chance of side effects if you’re not careful.
Dosage Limits Are Not Suggestions
The label says: “Do not take more than 6 tablets in 24 hours.” That’s not a suggestion. It’s a hard limit. For ibuprofen, the maximum daily dose for OTC use is 1,200 mg. That’s six 200 mg tablets. For naproxen, it’s 600 mg - that’s two 300 mg tablets, or three 220 mg tablets. But here’s what most people don’t realize: the 660 mg you get from three 220 mg tablets is already over the official 600 mg safety threshold. Many people think, “I’m just taking one extra pill for extra pain.” That’s how hospitalizations start.
A 2024 FDA report tracked a 68-year-old man who took the maximum OTC dose of naproxen for 14 straight days. He didn’t have any prior health issues. He just wanted to manage his arthritis. He ended up in the ER with acute kidney injury. The FDA’s own data shows that exceeding the 10-day limit - even by a few days - triples your risk of serious complications.
The Hidden Cardiovascular Risk
Everyone knows NSAIDs can upset your stomach. But few know they can trigger a heart attack - even in people with no history of heart disease.
In 2020, the FDA strengthened warnings for all non-aspirin NSAIDs after reviewing data from over 1.9 million patients. The risk isn’t theoretical. It’s real. And it can show up within the first week of use. Studies show that taking ibuprofen at high doses (1,500 mg or more daily) increases heart failure risk by 61%. Naproxen? Around 20%. That’s why the American Heart Association now says: if you have heart disease, avoid NSAIDs entirely - unless your doctor says otherwise.
Here’s the twist: naproxen may be slightly safer for your heart than ibuprofen. A 2015 FDA review found it had the most favorable cardiovascular profile among common NSAIDs. But that doesn’t mean it’s safe. It just means it’s less dangerous than the others. And if you’re over 65, have high blood pressure, or are on blood thinners? Neither one is safe without medical supervision.
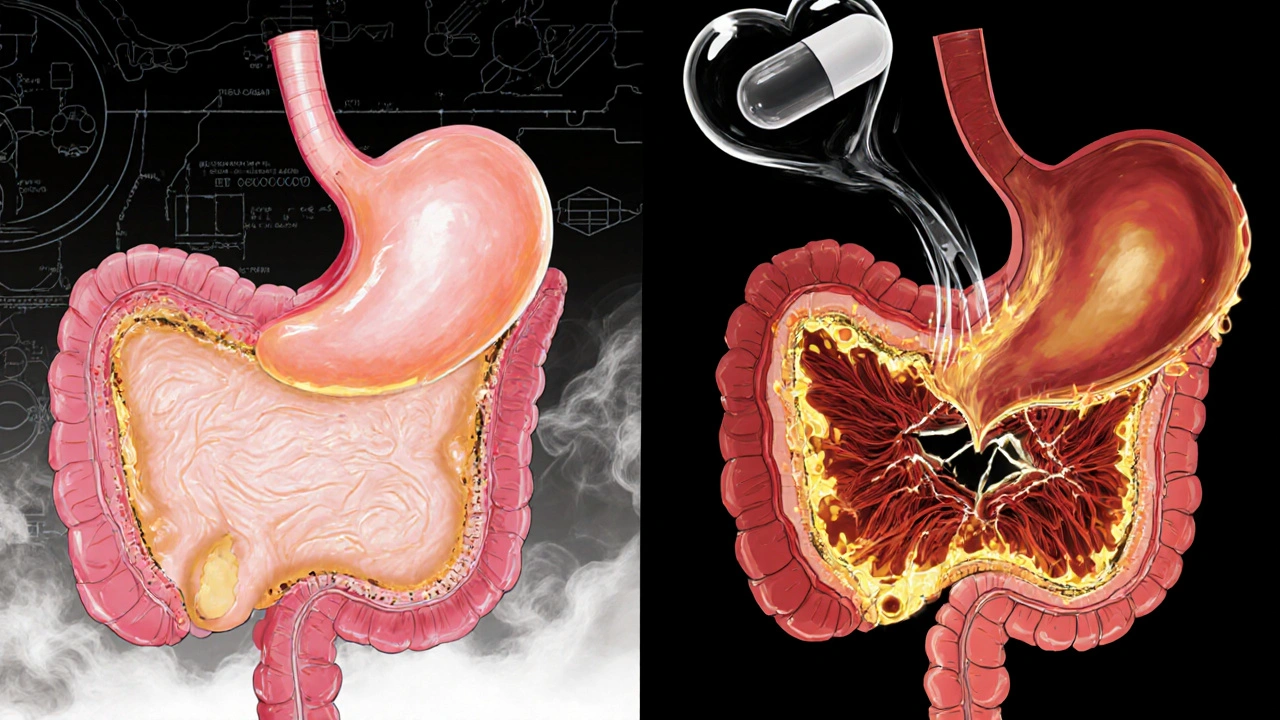
Stomach Problems Are More Common Than You Think
One in five people who take OTC NSAIDs regularly will develop stomach irritation. One in ten will develop an ulcer. And one in fifty will need hospital treatment for bleeding.
It’s not just “a little heartburn.” NSAIDs weaken the protective mucus layer in your stomach. Without it, acid eats away at the tissue. The damage builds slowly. You might feel fine for weeks. Then, one day, you wake up vomiting blood. That’s not a scare tactic. That’s a real outcome documented in the British Medical Journal and confirmed by the American College of Gastroenterology, which reports a 17% yearly rise in NSAID-related hospitalizations since 2018.
Reddit threads are full of stories like this: “Took 800 mg ibuprofen daily for months for back pain. Ended up with ulcers. Needed a scope. Missed two weeks of work.” Or: “I thought 200 mg was harmless. Took it every 4 hours for 10 days. Ended up in the ER with internal bleeding.” These aren’t outliers. They’re predictable.
Who Should Never Take These Pills
There are nine groups of people who should avoid NSAIDs entirely unless a doctor says otherwise:
- People with kidney disease - NSAIDs reduce blood flow to the kidneys.
- People with heart failure or high blood pressure - they can cause fluid retention and worsen heart strain.
- People with a history of stomach ulcers or bleeding - NSAIDs make bleeding much more likely.
- Pregnant women - especially after 20 weeks - NSAIDs can cause low amniotic fluid and fetal kidney problems.
- People over 65 - age increases sensitivity to side effects.
- People taking blood thinners like warfarin or aspirin - NSAIDs can cause dangerous bleeding.
- People with asthma - NSAIDs can trigger severe asthma attacks in some.
- People with liver disease - NSAIDs can worsen liver damage.
- Children and teens with viral infections - NSAIDs can increase the risk of Reye’s syndrome, a rare but deadly condition.
If you fall into any of these categories, acetaminophen (paracetamol) is usually the safer choice - but even that has limits. Don’t exceed 3,000 mg per day. Liver damage from acetaminophen is silent until it’s too late.

What You Should Do Instead
NSAIDs aren’t evil. They’re useful - when used correctly. But they’re not meant for daily, long-term pain. If you’re taking them for more than 10 days, you’re not treating the problem. You’re masking it.
Ask yourself: Why do I need this painkiller every day? Is it a pinched nerve? Arthritis? Stress? The CDC’s 2022 guidelines say: for chronic pain, non-drug treatments should come first. Physical therapy. Stretching. Heat packs. Weight management. Even walking 20 minutes a day reduces joint pain more effectively than daily ibuprofen.
For short-term relief? Fine. Take one tablet with food. Don’t take it on an empty stomach. Don’t mix it with alcohol. Don’t take it longer than 10 days. And if you feel dizzy, swollen, or notice dark stools? Stop immediately. Call your doctor. Don’t wait.
What the Label Doesn’t Tell You
Most people don’t read the Drug Facts label. A 2023 survey found that only 28% of consumers read the entire label on OTC pain meds. That’s shocking. The label tells you:
- Maximum daily dose
- When not to use it
- What to avoid mixing it with
- How long to use it
And here’s one thing no one talks about: ibuprofen can block the heart-protective effect of low-dose aspirin. If you’re taking aspirin to prevent a heart attack, taking ibuprofen at the same time can cancel out its benefits. Naproxen doesn’t do this as much - but it’s still risky. The fix? Take aspirin at least 30 minutes before ibuprofen, or space them 8 hours apart. If you’re unsure, talk to your pharmacist.
Bottom Line: Use Smart, Not Often
NSAIDs are powerful tools. But they’re not candy. They’re not harmless. They’re not “just painkillers.” They’re drugs with real, documented risks - and most people have no idea how serious those risks are.
Here’s what you need to remember:
- Never exceed 1,200 mg of ibuprofen or 600 mg of naproxen in 24 hours.
- Don’t use OTC NSAIDs for more than 10 days straight without seeing a doctor.
- Take them with food. Never on an empty stomach.
- If you have heart, kidney, stomach, or liver issues - avoid them unless your doctor says it’s okay.
- For chronic pain, try movement, heat, or physical therapy before reaching for the bottle.
- Always read the label. If you don’t understand it, ask your pharmacist.
There’s no magic pill for pain. But there is a smarter way to manage it - one that doesn’t risk your heart, your stomach, or your kidneys.
Can I take ibuprofen and naproxen together?
No. Never take ibuprofen and naproxen together. They’re both NSAIDs, and combining them doesn’t give you better pain relief - it just doubles your risk of stomach bleeding, kidney damage, and heart problems. If one isn’t working, talk to your doctor. Don’t stack them.
Is naproxen safer than ibuprofen for the heart?
Yes, according to FDA analyses, naproxen has a slightly lower risk of causing heart attacks and strokes compared to ibuprofen. But that doesn’t mean it’s safe. Both carry serious cardiovascular warnings. If you have heart disease, avoid both unless your doctor specifically approves one.
How long can I safely take OTC NSAIDs?
No longer than 10 days in a row. That’s the official limit from the FDA, NHS, and Mayo Clinic. If your pain lasts longer, it’s a sign you need to see a doctor - not take more pills. Chronic pain needs diagnosis, not just masking.
Can I take NSAIDs if I’m on blood pressure medication?
Be very careful. NSAIDs can make blood pressure medications less effective and may cause your blood pressure to rise. They can also reduce blood flow to the kidneys, which is dangerous if you’re already on diuretics or ACE inhibitors. Always check with your doctor before using them.
Is acetaminophen safer than NSAIDs?
For most people, yes. Acetaminophen doesn’t cause stomach ulcers or increase heart risk like NSAIDs do. But it can damage your liver if you take more than 3,000 mg per day - especially if you drink alcohol or have liver disease. It’s safer for your stomach and heart, but not risk-free.
What should I do if I accidentally took too much?
If you took more than the maximum daily dose - even just one extra pill - stop taking it immediately. Watch for signs like nausea, vomiting, dizziness, dark stools, or swelling in your legs. If you feel unwell or are unsure, call Poison Control or go to the ER. Don’t wait for symptoms to get worse.

Aidan McCord-Amasis
November 15, 2025 AT 12:42NSAIDs are literally candy for adults now 😅
Katie Baker
November 15, 2025 AT 15:25I used to take ibuprofen like it was gum until I got a stomach bleed. Now I stretch, ice it, and just breathe through the pain. Best decision ever.
Also, my grandma swears by a heating pad and CBD cream. Not magic, but way safer than pills.
Thanks for posting this - I wish I’d seen it 5 years ago.
Hollis Hollywood
November 16, 2025 AT 12:50I read this whole thing and just sat there quietly, thinking about how many people I know who’ve been popping these like Skittles.
My cousin took naproxen every day for his back pain for over a year. He didn’t even know he had high blood pressure until he ended up in the hospital. They found kidney scarring. He’s 42.
I’ve started asking people, ‘Hey, are you taking anything for that pain?’ - not to judge, just to make sure they know what they’re doing. It’s scary how little people are told. The labels are practically invisible. And the ads? ‘Feel better in minutes!’ No mention of the silent damage.
I used to think if it was OTC, it was safe. Now I see it’s just… accessible. That’s not the same thing.
Also, I didn’t know ibuprofen could cancel out aspirin. I take low-dose aspirin for my heart. I’ve been taking Advil for headaches. I’m switching to Tylenol now. Thanks for the wake-up call.
It’s not about fear. It’s about awareness. And this post? It’s the kind of thing that actually saves lives. Not just because of the facts, but because someone finally said it plainly. No fluff. No marketing. Just truth.
I’m gonna share this with my family. Everyone needs to see this.
John Foster
November 18, 2025 AT 02:22There’s a deeper truth here, buried beneath the dosage charts and FDA warnings - we’ve turned our bodies into machines that need constant calibration, and painkillers are the lubricant we pour into the gears until they seize.
We don’t ask why the pain exists. We don’t sit with it. We don’t listen to what our bodies are screaming. We just silence it with chemistry. And then we wonder why we’re always tired, why our digestion is off, why our anxiety spikes.
The pharmaceutical industry didn’t invent pain. But they did invent the illusion that pain can be erased without consequence. And now we’re paying the price - not just in kidney failure and ulcers, but in the slow erosion of our relationship with our own flesh.
What if pain isn’t the enemy? What if it’s the last honest thing left in a world of synthetic comfort?
I’m not saying suffer. I’m saying: feel. Then act. Not with a pill. With awareness.
And if you’re still reading this, congratulations. You’re one of the few who didn’t scroll past. That’s the first step.
Edward Ward
November 18, 2025 AT 11:18Just to clarify - naproxen’s cardiovascular risk is lower than ibuprofen’s, but it’s still elevated compared to placebo, right? Yes. And the 2015 FDA meta-analysis showed that, but also noted that naproxen’s longer half-life means cumulative exposure is higher with chronic use - so even if per-dose risk is lower, total exposure may negate that advantage.
Also, the 660 mg vs. 600 mg naproxen threshold? That’s a real trap. Many brands sell 220 mg tablets and say ‘take three’ - which is 660 mg. The FDA label says 600 mg max. So technically, even ‘recommended’ use is over the limit. That’s not a typo - that’s a regulatory loophole.
And the aspirin interaction? Critical. People on daily aspirin for cardiac protection are often unaware that ibuprofen can block its antiplatelet effect for up to 8 hours. Taking ibuprofen 30 minutes before aspirin? That’s the only safe window. But who reads that? No one.
And acetaminophen? Liver toxicity is silent. You can take 4,000 mg a day for months, feel fine, then one day - boom - ALT levels sky-high. No warning signs. No pain. Just death in slow motion.
This isn’t just about pills. It’s about how we’ve outsourced bodily autonomy to corporations and convenience. The label is there. We just choose not to see it.
And yet - I still take ibuprofen sometimes. I’m not perfect. But now I know. And that changes everything.
Jessica Chambers
November 19, 2025 AT 18:29So… you’re saying I shouldn’t take two Advil for my period? 😏
Wow. I’m devastated. My whole life was a lie.
JK. But seriously - this is the most useful thing I’ve read all month. Thank you.
Also, I now know why my last ER visit was so awkward when I told them I ‘just took a few extra pills.’ They looked at me like I’d admitted to eating a whole cake in one sitting.
Reading the label = adulting level: expert.
Adam Dille
November 20, 2025 AT 00:00Man, I feel like this should be required reading in high school. Like right after sex ed and before driver’s ed.
I used to think if it’s on the shelf next to gum and candy, it’s harmless. Now I know it’s more like a loaded gun with a sticker that says ‘use responsibly.’
My mom’s on blood pressure meds and takes naproxen for her knees. I’m sending her this. She’s gonna roll her eyes, but she’ll read it.
Also - heat pack > pill. Just saying.
And yeah, I’m gonna start asking my friends: ‘What are you taking for that?’ instead of just nodding and saying ‘yeah, I know, pain sucks.’
Thanks for writing this. It’s the kind of post that makes you pause and think - not just scroll.
Shyamal Spadoni
November 20, 2025 AT 19:01Did you know the FDA is controlled by Big Pharma? They only say these things to scare you so you buy more expensive prescriptions
NSAIDs are natural and have been used for centuries - aspirin came from willow bark
They just want you dependent on doctors and pills
My cousin in Nigeria takes ibuprofen every day and he’s 89 and still lifts goats
Trust your body not the government
Also the label says 6 tablets but I take 8 and I’m fine
They don’t want you to know this
Just sayin'
Ogonna Igbo
November 21, 2025 AT 23:23You Americans think everything is dangerous because you are weak
In Nigeria we take 10 tablets of naproxen for fever and go to work
Why you always need doctor to tell you what to do
My uncle took ibuprofen for 20 years and he still run market
You are too soft
Let people choose
Stop scare tactics
This is why Africa is stronger than USA
Real men don't read labels
Andrew Eppich
November 22, 2025 AT 05:11It is regrettable that the public discourse surrounding over-the-counter pharmaceuticals has devolved into a spectacle of emotional appeals and anecdotal testimony. The data presented here is, in fact, statistically significant and empirically validated by multiple peer-reviewed studies and regulatory agencies. To dismiss these findings as fearmongering is not merely irresponsible - it is a failure of civic literacy.
The fact that individuals continue to exceed recommended dosages, ignore contraindications, and conflate accessibility with safety reflects a broader societal decline in critical thinking. One does not become an expert on pharmacology by reading Reddit threads - one becomes an expert by consulting peer-reviewed literature, clinical guidelines, and pharmacokinetic profiles.
It is not the fault of the medication. It is the fault of the user who chooses ignorance over information. And yet, the blame is always assigned to the label, the manufacturer, or the FDA - never to the individual who refuses to read.
This is not a crisis of pharmaceutical safety. This is a crisis of personal accountability.
And if you still think you are entitled to pain relief without consequence - then perhaps you should not be allowed to purchase these substances at all.