
Stroke Recovery Support Planner
Acute Phase (0-2 weeks)
Focus on safety, basic mobility, and initial therapy.
- Assist with transfers and gentle ankle pumps
- Practice simple naming games
- Provide reassurance and maintain calm environment
Sub-Acute Phase (3-12 weeks)
Build strength and confidence with structured therapy.
- Practice sit-to-stand and short walks
- Encourage reading aloud and memory drills
- Introduce peer support meetings and short outings
Long-Term Phase (3+ months)
Focus on reintegration and preventing future strokes.
- Increase walking distance and balance exercises
- Practice complex conversations and problem-solving
- Encourage independent hobbies and regular therapy reviews
Daily Care Checklist
Use this checklist to ensure consistent care throughout the day:
- Morning: Check vitals, administer medications, assist with bathroom routine
- Mid-day: Review therapy exercises, monitor nutrition
- Afternoon: Conduct speech practice, encourage mobility
- Evening: Review medication list, assess pain levels
- Night: Ensure safe sleep environment, set alarms for next-day meds
Keep this list visible for easy reference!
Home Safety Tips
- Place non-slip mats in bathrooms and kitchens
- Install grab bars near toilets and showers
- Raise bed height with sturdy platform
- Keep walkways clear of rugs and clutter
Emotional Support Strategies
- Listen without trying to fix feelings
- Encourage short social interactions
- Introduce mindfulness or breathing exercises
- Refer to neuropsychologist if needed
Caregiver Self-Care Reminder
Remember: A healthy caregiver is the strongest pillar of the recovery team.
- Schedule 30 minutes of personal downtime daily
- Stay connected with your support circle
- Consider monthly respite stays
When a family member experiences a stroke, the road ahead feels unclear and overwhelming. You want to help, but you aren’t sure what to do, when to step in, or how to keep your own sanity intact. This guide walks you through the most important actions you can take, from the first days at home to long‑term rehabilitation, so you can be a steady, effective presence in your loved one’s recovery journey.
- Know the three recovery phases and what support looks like at each stage.
- Learn concrete daily tasks that boost physical, speech, and emotional healing.
- Get a quick‑reference checklist for home safety and medication management.
- Find out how to tap into professional services and community resources.
- Protect your own well‑being while caring for someone else.
What Exactly Is a Stroke?
Stroke is a sudden interruption of blood flow to the brain, either by a clot (ischemic) or a burst vessel (hemorrhagic). The damage can affect movement, speech, memory, and emotions, depending on which brain area is hit. About 15million people worldwide suffer a stroke each year, and roughly one‑third never regain full independence.
Who Is the Caregiver?
Caregiver refers to the family member or friend who provides day‑to‑day assistance during recovery. You become the bridge between medical professionals and the patient, handling appointments, medication, and emotional encouragement.
Understanding the Recovery Timeline
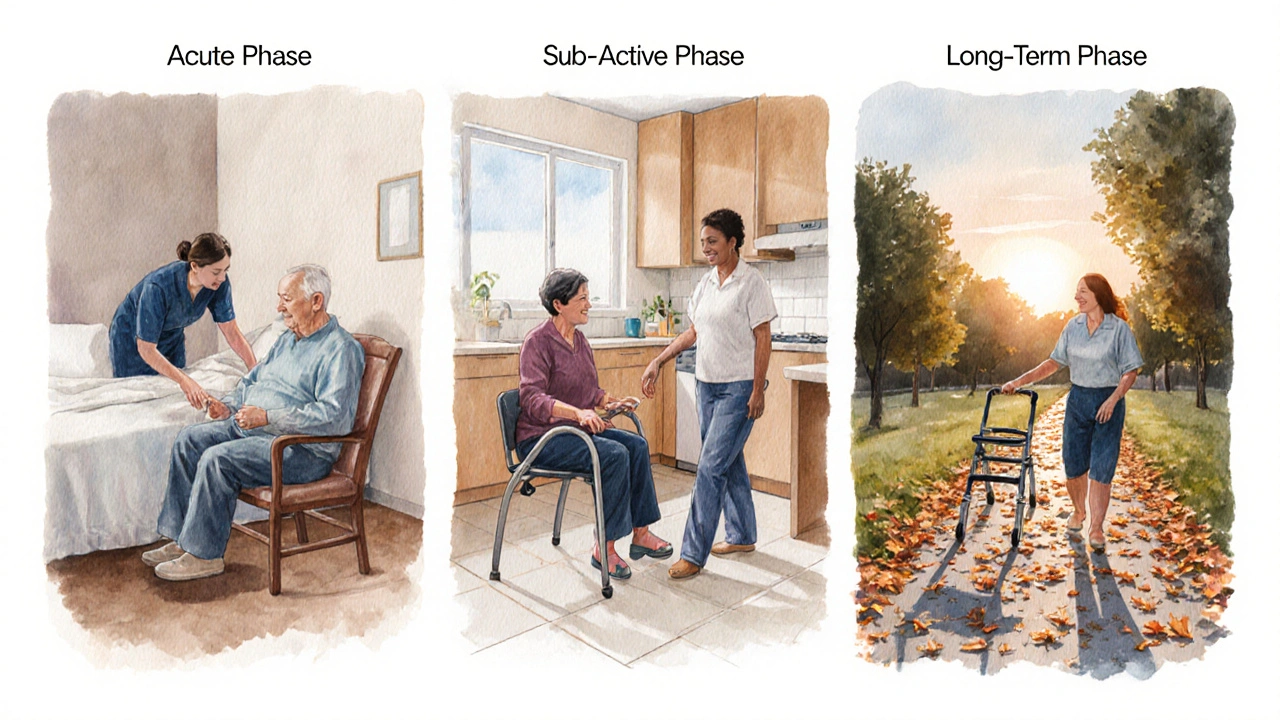
Recovery typically unfolds in three overlapping phases:
- Acute phase (first 1‑2 weeks): Hospital discharge, establishing safety at home, and beginning basic therapy.
- Sub‑acute phase (weeks 3‑12): More intensive rehab, goal‑oriented exercises, and rebuilding confidence.
- Long‑term phase (months to years): Community reintegration, fine‑tuning skills, and preventing secondary strokes.
Each stage calls for different levels of physical, speech, and emotional support.
Physical Rehabilitation Basics
Physical therapy focuses on restoring strength, balance, and mobility is the backbone of early recovery. Your role includes:
- Ensuring the therapist’s home‑exercise plan is followed twice daily.
- Monitoring fatigue: stop if the patient’s heart rate spikes above 120bpm or they become breathless.
- Using simple tools-resistance bands, a stable chair, and a walker-to practice sit‑to‑stand moves.
Research from the American Stroke Association (2023) shows that patients who repeat therapist‑prescribed exercises at least 5times a day improve walking speed by 30% more than those who don’t.
Speech and Cognitive Therapy
Speech therapy addresses language, swallowing, and cognitive deficits after stroke often starts while the patient is still in the hospital. At home, you can:
- Practice naming objects: lay out three items and ask the patient to label them.
- Encourage reading aloud for 10 minutes, then discuss the story to stimulate comprehension.
- Use safe swallowing exercises recommended by the therapist, like holding a small sip of water and swallowing twice.
Engaging in these activities daily can shorten the average speech‑rehab timeline from 12 weeks to about 8 weeks.
Occupational Therapy and Daily Living
Occupational therapy helps patients relearn everyday tasks such as dressing, cooking, and bathing. Support tips:
- Break tasks into tiny steps-e.g., for dressing: first locate the shirt, then orient it inside out, finally pull over the head.
- Use adaptive equipment: button hooks, built‑in grips on utensils, and shower chairs.
- Celebrate every successful step to reinforce confidence.
Medication Management
Medication includes antiplatelets, anticoagulants, blood‑pressure drugs, and cholesterol‑lowering agents prescribed after a stroke. Errors are common, so set up a system:
- Use a weekly pill organizer labeled by day and time.
- Keep a medication list on the fridge: drug name, dosage, purpose, and prescribing doctor.
- Set phone alarms for each dose and double‑check with a pharmacy‑provided medication chart.
Studies in 2024 found that patients with a dedicated caregiver reduced medication‑related readmissions by 42%.
Emotional and Psychological Support
The brain injury often triggers anxiety, depression, and frustration. As a caregiver, you can:
- Listen without trying to “fix” the feeling-just acknowledge, "I hear how hard this is for you."
- Encourage short, frequent social interactions: a 15‑minute video call with a friend can lift mood.
- Introduce mindfulness or breathing exercises for stress reduction, using apps that guide a 5‑minute session.
When emotional distress is severe, ask the neurologist about a referral to a neuropsychologist. Early counseling cuts the risk of post‑stroke depression by half.
Adapting the Home Environment
Home modifications are changes made to reduce fall risk and improve accessibility after stroke can be simple yet powerful:
- Place non‑slip mats in the bathroom and kitchen.
- Install grab bars next to the toilet and shower.
- Raise the height of the bed by a few inches with a sturdy platform.
- Keep a clear pathway: remove loose rugs and clutter from main walkways.
A 2022 Home Safety Study showed that these low‑cost modifications lowered in‑home falls by 35% for stroke survivors.
Building a Support Network
Going solo isn’t sustainable. Tap into these resources:
- Support groups: Local chapters of the American Stroke Association meet monthly; they provide peer advice and emotional relief.
- Home‑health agencies: Certified nursing assistants can assist with dressing, bathing, and wound care.
- Respite services: Many nonprofits offer a few hours of free caregiver relief each week.
- Online forums: Websites like StrokeRecovery.org host discussion boards where families share tips.
Having at least one trusted person you can call when you’re exhausted reduces caregiver burnout by 47%.
Quick Reference: Support Activities by Recovery Phase
| Recovery Phase | Key Physical Tasks | Speech & Cognitive Focus | Emotional Support |
|---|---|---|---|
| Acute (0‑2weeks) | Assist transfers, encourage gentle ankle pumps | Simple naming games, swallow checks | Provide reassurance, keep environment calm |
| Sub‑acute (3‑12weeks) | Practice sit‑to‑stand, short walks with a walker | Reading aloud, memory recall drills | Introduce peer‑support meetings, schedule short outings |
| Long‑term (3months+) | Increase walking distance, balance exercises | Complex conversation practice, problem‑solving tasks | Encourage independent hobbies, maintain regular therapy reviews |
Daily Care Checklist for Caregivers
- Morning: Check vitals, administer medications, assist with bathroom routine.
- Mid‑day: Review therapy exercises, monitor nutrition (focus on protein‑rich meals).
- Afternoon: Conduct speech practice, encourage a short walk or seated mobility drill.
- Evening: Review medication list, assess pain levels, provide emotional check‑in.
- Night: Ensure safe sleep environment, set alarms for next‑day meds, document any changes for the doctor.
Keep this list on the fridge and tick off each item; consistency builds trust and speeds recovery.
Take Care of Yourself, Too
Burnout silently erodes the quality of care you can give. Apply the same principles you use for your loved one:
- Schedule 30minutes of personal downtime each day-read, walk, or practice a hobby.
- Stay connected with your own support circle; share frustrations openly.
- Consider a short‑term respite stay once a month; a refreshed mind equals better support.
Remember, a healthy caregiver is the strongest pillar of the recovery team.

Frequently Asked Questions
How soon should I start home exercises after a stroke?
Most therapists recommend gentle, assisted movements within 24‑48hours of hospital discharge, as long as the patient’s vital signs are stable. Start with range‑of‑motion stretches and progress under professional guidance.
What signs indicate a medication error?
Look for new dizziness, unexpected bruising, confused speech, or a sudden change in blood pressure. If any of these appear, contact the prescribing doctor immediately.
Can I safely lift my loved one without a back injury?
Use your legs, not your back: bend at the knees, keep the spine straight, and keep the person close to your body. If they weigh more than 20kg, get a transfer board or ask a second person to help.
When should I involve a speech‑language pathologist?
If the patient shows any trouble forming words, swallowing, or understanding simple instructions within the first week, a referral to a speech‑language pathologist is recommended.
How can I prevent another stroke?
Control blood pressure, maintain a low‑salt diet, stay active, take prescribed antiplatelet or anticoagulant medication, and avoid smoking. Regular check‑ups with the neurologist keep the risk under watch.

HAMZA JAAN
October 3, 2025 AT 18:25Look, the first two weeks are all about keeping the survivor safe and not over‑doing it. Simple things like ankle pumps and gentle transfers can stop a lot of secondary complications. Keep the environment calm; loud arguments or sudden noises can spike blood pressure. And remember, you’re not a nurse – just a steady presence who can hand over the meds and a reassuring smile.
April Rios
October 3, 2025 AT 23:58From a philosophical angle, the acute phase mirrors the concept of “beginning again” – the brain is rebooting, and the caregiver’s role is to provide a scaffold of stability while neuroplasticity does its work. This mindset helps prevent you from feeling like you’re “fixing” everything, and instead you become a facilitator of the patient’s own recovery pathways.
byron thierry
October 4, 2025 AT 05:32When dealing with stroke recovery, consistency outweighs intensity; six short sessions of guided movement across a day usually beat a single marathon workout. You want to schedule sit‑to‑stand drills in the morning, a brief walk after lunch, and a balance exercise before dinner. The key is to observe fatigue cues – if the heart rate jumps above 120 bpm or the patient sighs heavily, pause and let them rest. In the speech arena, naming three objects around the kitchen each hour reinforces language circuits without overwhelming the brain. Reading aloud for ten minutes, then asking the patient to summarize the plot, trains both comprehension and expressive abilities. Swallowing exercises, like the “two‑sip” technique, should be practiced with a therapist‑approved water volume to keep aspiration at bay. Medication management is more than a pillbox; it’s a ritual that signals to the brain that the body is under control, reducing anxiety. Set alarms on two separate devices – a phone and a kitchen timer – to double‑check doses. Document any side effects in a notebook that you share with the neurologist at each appointment. Home safety is a low‑cost investment: non‑slip mats and grab bars can cut fall risk by a third, according to recent studies. Keep pathways clear, especially the route from bedroom to bathroom, because night‑time trips are the most dangerous. Emotional support isn’t just “listen”; it’s validating the frustration of lost abilities while highlighting any tiny triumphs, like gripping a spoon. Encourage social interaction, even a five‑minute video call, because isolation accelerates depressive symptoms. If depression signs appear – persistent sadness, loss of appetite, or hopelessness – push for a neuropsychology referral without delay. Finally, never neglect your own wellbeing; a caregiver who sleeps, eats, and exercises is the most reliable anchor for the patient’s ongoing recovery.
bob zika
October 4, 2025 AT 11:05It is imperative, therefore, to acknowledge the multifaceted nature of post‑stroke care, encompassing physical therapy, speech rehabilitation, medication adherence, and psychosocial support, each of which synergistically contributes to optimal outcomes; moreover, the integration of structured daily checklists, environmental modifications, and professional consultations, when executed with diligence and regularity, markedly reduces the probability of complications, including falls, medication errors, and secondary depressive episodes.
M Black
October 4, 2025 AT 16:38Take a 30‑minute walk each day; it boosts mood and circulation 😊
Joanne Myers
October 4, 2025 AT 22:12The caregiver’s self‑care regimen must include regular respite, adequate nutrition, and mental health monitoring to sustain long‑term effectiveness.
rahul s
October 5, 2025 AT 03:45Indeed, scheduling a weekly coffee break with a trusted friend or a brief yoga session can recharge mental reserves, and these micro‑breaks are scientifically linked to decreased burnout rates among caregivers.
Julie Sook-Man Chan
October 5, 2025 AT 09:18Keeping the bedroom free of clutter prevents nighttime trips to the bathroom from turning into accidents.
Amanda Mooney
October 5, 2025 AT 14:52Also, consider placing night‑lights along the hallway; a soft illumination guides the patient without disrupting sleep cycles.
Tommy Mains
October 5, 2025 AT 20:25Use a weekly pill organizer labeled with both day and time; it eliminates guesswork and ensures each medication is taken exactly as prescribed.
Danielle Ryan
October 6, 2025 AT 01:58But beware, the pharmaceutical industry often hides side‑effects behind glossy brochures, and without vigilant monitoring you might be unwittingly feeding the very system that caused the initial stroke!
Robyn Chowdhury
October 6, 2025 AT 07:32The article is thorough, yet it could benefit from more visual aids to illustrate home‑modification steps. 🤔
Deb Kovach
October 6, 2025 AT 13:05Good point – a simple diagram of grab‑bar placement or a checklist graphic would make the guidance instantly actionable for visual learners.
Sarah Pearce
October 6, 2025 AT 18:38i think the section on speech therapy could use more real‑life examples, like naming games that actually work, not just vague suggestions.
Daisy Aguirre
October 7, 2025 AT 00:12Absolutely! Try the “kitchen cabinet” game: place three common items on a shelf and ask the survivor to name them while you time the response – it’s fun, practical, and reinforces neural pathways.