Decongestant Safety Checker
Medication Safety Check
Check if your blood pressure medication interacts with nasal decongestants
Result
Note: This is for informational purposes only. Always consult your doctor before using any medication.
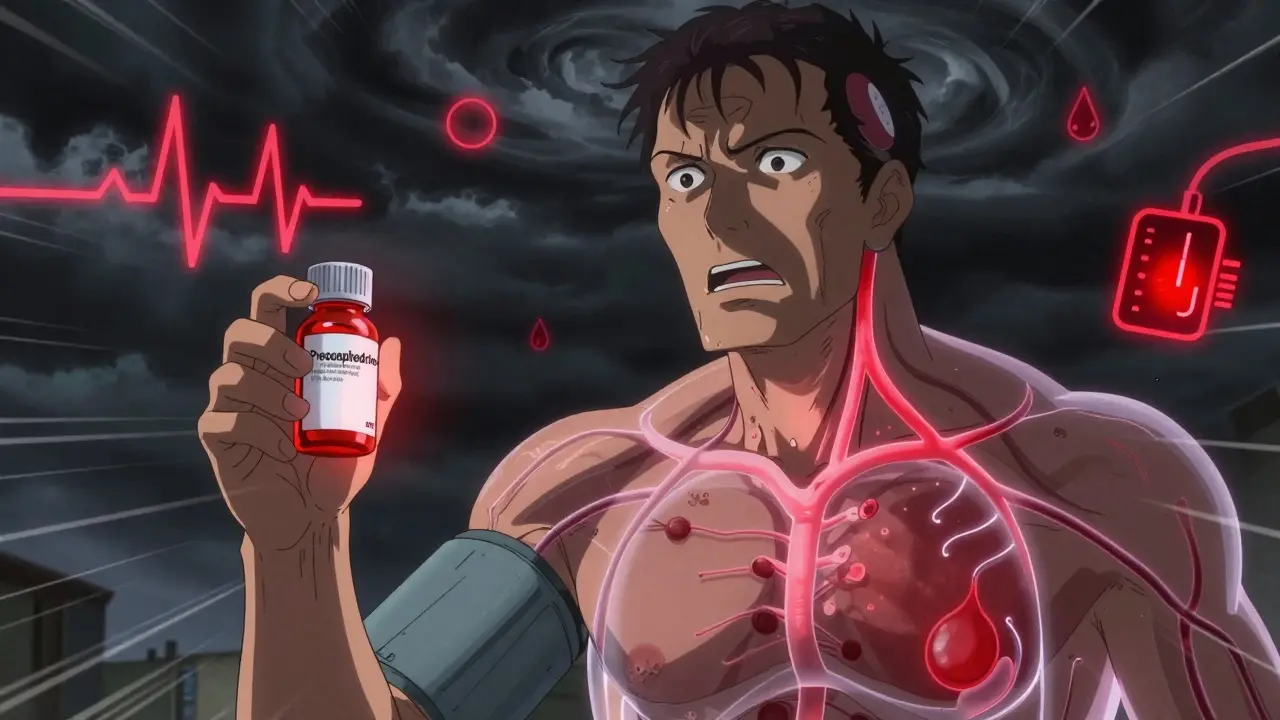
If you’re on blood pressure medication and get a stuffy nose, you might reach for a nasal decongestant without thinking twice. But here’s the truth: that little bottle could be hiding a serious risk. Many over-the-counter decongestants can spike your blood pressure, undo the work of your prescription meds, or even trigger a heart-related emergency. This isn’t just a warning on a label-it’s a real, documented danger affecting millions.
How Decongestants Raise Blood Pressure
Nasal decongestants like pseudoephedrine and phenylephrine work by tightening blood vessels in your nose to reduce swelling. That’s why your nose clears up fast. But here’s the catch: those same blood vessels are everywhere-in your heart, brain, kidneys, and limbs. When the medicine tightens them systemically, your blood pressure rises. It’s not a small bump. Studies show pseudoephedrine can increase systolic blood pressure by 2 to 5 mmHg on average, and sometimes much more in sensitive individuals. For someone with uncontrolled hypertension, that’s enough to push them into danger zone.Even topical sprays like oxymetazoline (found in Afrin) aren’t safe. Many people think since it’s sprayed in the nose, it stays local. But research from the University of Michigan Health System shows about 30% of the active ingredient can enter your bloodstream. That’s enough to trigger palpitations, dizziness, or a sudden spike in pressure. The American Heart Association has been clear since 2023: if you have high blood pressure, don’t use these without talking to your doctor first.
Which Blood Pressure Medications Are at Risk?
It’s not just about having high blood pressure-it’s about what you’re taking to control it. Decongestants interfere with several common classes of antihypertensive drugs:- Beta-blockers like metoprolol and atenolol: Decongestants can override their ability to slow your heart rate, leading to rapid or irregular heartbeat.
- Calcium channel blockers like felodipine and nifedipine: These help relax blood vessels, but decongestants force them to tighten again, making the drug less effective.
- ACE inhibitors and ARBs: While less directly affected, decongestants can still cause fluid retention and raise pressure, countering their benefits.
- Diuretics: Some decongestants contain hidden sodium, which cancels out the fluid-reducing effect of water pills.
A 2024 study in the Journal of Clinical Hypertension found that over 22% of emergency visits for uncontrolled high blood pressure in adults over 50 were linked to people using OTC decongestants without knowing the risk. That’s not rare-it’s common.
Hidden Decongestants in Cold and Flu Products
One of the biggest traps? You don’t even know you’re taking a decongestant. Many cold, flu, and allergy meds combine multiple ingredients. A bottle labeled “Sinus Relief” or “All-in-One Cold & Flu” might contain phenylephrine or pseudoephedrine right under the surface.Check the “Active Ingredients” list-not the front label. Look for these names:
- Pseudoephedrine
- Phenylephrine
- Oxymetazoline
- Ephedrine
- Dimethylaminoethanol (DMAE)
Even “non-drowsy” formulas often hide decongestants. If you’re on blood pressure meds, never assume a product is safe just because it says “for sensitive users.” A 2024 survey by the Cleveland Clinic found only 38% of hypertension patients could correctly identify decongestants as risky. That’s a dangerous gap.

What to Use Instead
You don’t need decongestants to feel better. Several safe, effective alternatives exist:- Nasal saline spray: Plain saltwater rinses (like NeilMed or store-brand saline) flush out mucus without affecting blood pressure. Use 2-3 times a day.
- Humidifiers and steam: A hot shower or bowl of hot water with a towel over your head helps open nasal passages naturally. Add a drop of eucalyptus oil if you like-it’s safe and soothing.
- Antihistamines: If your congestion comes from allergies (not a cold), loratadine (Claritin) or cetirizine (Zyrtec) are safe for most people on blood pressure meds. They don’t constrict blood vessels.
- Elevating your head: Sleep with an extra pillow. Gravity helps drain sinuses overnight.
These won’t work as fast as a decongestant, but they work safely. And they don’t risk a heart attack.
When You Absolutely Must Use a Decongestant
Sometimes, the risk is unavoidable. If your doctor says it’s okay to use a decongestant for a few days, follow these rules:- Use the lowest dose possible-never double up.
- Take it for no more than 3 days. Longer use raises the risk of rebound congestion and dangerous pressure spikes.
- Check your blood pressure twice a day while using it. If it rises more than 15 points from your normal baseline, stop immediately and call your doctor.
- Never use it if you have heart disease, irregular heartbeat, or uncontrolled hypertension-even if your doctor says yes, be extra cautious.
And remember: pseudoephedrine is kept behind the pharmacy counter in the U.S. for a reason. That’s not to inconvenience you-it’s so the pharmacist can ask if you’re on blood pressure meds. Use that moment. Ask them: “Is this safe with my lisinopril and metoprolol?”
Why Pharmacists Are Your Secret Weapon
Pharmacists aren’t just people who hand out pills. They’re trained to catch dangerous interactions. A study in the Journal of the American Pharmacists Association showed that when pharmacists proactively reviewed patients’ medications, inappropriate decongestant use dropped by 47%. That’s huge.Bring your full list of meds-prescription, OTC, vitamins, supplements-to the pharmacy every time you pick something up. Say: “I’m on blood pressure meds. Can you check if this is safe?” Most pharmacists will do it for free. Don’t be shy. This is exactly why they’re there.

What to Watch For
If you accidentally take a decongestant while on blood pressure meds, watch for these signs:- Headache or pounding in your temples
- Fast or irregular heartbeat
- Blurred vision
- Chest tightness or pain
- Dizziness or fainting
If you feel any of these, stop the decongestant immediately. Drink water. Sit down. Check your blood pressure. If it’s above 180/110 or you have chest pain, call emergency services. Don’t wait. This isn’t something to “see if it passes.”
Long-Term Strategy: Know Your Meds
The best way to avoid this problem? Stay informed. Keep a written list of every medication you take, including doses and why you take them. Update it every time your doctor changes something. Show it to every new provider-even your dentist or urgent care doctor.Also, be wary of sodium in cold medicines. The American Heart Association warns that some OTC products contain over 200 mg of sodium per dose-enough to raise blood pressure in salt-sensitive people. Look for “sodium-free” labels, or ask your pharmacist.
There’s hope on the horizon. As of 2025, several pharmaceutical companies are testing new decongestants that don’t affect blood vessels at all. But until those are widely available, stick to the safe choices.
Final Rule: When in Doubt, Skip It
Your blood pressure matters more than a stuffy nose. Decongestants are not harmless. They’re powerful drugs with serious side effects-especially when mixed with heart meds. There are safer ways to breathe easier. Use them. Your heart will thank you.Can I use nasal saline spray if I have high blood pressure?
Yes, nasal saline spray is completely safe for people with high blood pressure. It works by flushing out mucus and irritants with saltwater and doesn’t affect blood vessels or heart function. Use it as often as needed-there’s no risk of rebound congestion or blood pressure spikes.
Is phenylephrine safer than pseudoephedrine for high blood pressure?
No, phenylephrine is not safer. While it’s less potent than pseudoephedrine, studies still show it can raise blood pressure, especially in sensitive individuals. Both are risky for people on blood pressure medication. Neither should be used without a doctor’s approval.
Can I take decongestants if my blood pressure is controlled?
Even if your blood pressure is well-controlled, decongestants can still cause dangerous spikes. Many people assume “controlled” means safe, but decongestants can override your meds. Always talk to your doctor before using them-even if you feel fine.
Do topical decongestant sprays like Afrin affect blood pressure?
Yes. Although applied locally, up to 30% of oxymetazoline (the active ingredient in Afrin) enters the bloodstream. This can raise blood pressure and cause heart palpitations. Avoid all nasal sprays with decongestants if you have high blood pressure.
What should I do if I accidentally took a decongestant?
Stop taking it immediately. Check your blood pressure. If it’s elevated (more than 15 points above your normal), rest, stay hydrated, and monitor for chest pain, dizziness, or rapid heartbeat. Call your doctor or go to urgent care if symptoms persist. Don’t wait for them to get worse.
Are there any OTC cold meds that are safe for high blood pressure?
Yes-but only if they contain no decongestants. Look for products labeled “for high blood pressure” or check the active ingredients. Safe options include plain antihistamines (like loratadine), pain relievers like acetaminophen (Tylenol), and saline sprays. Avoid anything with pseudoephedrine, phenylephrine, or oxymetazoline.

Beth Templeton
January 7, 2026 AT 04:56Rachel Wermager
January 8, 2026 AT 21:10Leonard Shit
January 10, 2026 AT 13:26Wesley Pereira
January 10, 2026 AT 14:34Isaac Jules
January 12, 2026 AT 13:24Stuart Shield
January 14, 2026 AT 05:43Gabrielle Panchev
January 14, 2026 AT 22:56Molly McLane
January 16, 2026 AT 05:34Katelyn Slack
January 17, 2026 AT 05:09