Angioedema Type Finder
This tool helps identify the likely type of angioedema based on your symptoms and triggers. It's not a substitute for professional medical diagnosis.
Symptoms & Triggers
Please select all symptoms and triggers you've experienced:
Diagnostic History
Recommended Angioedema Type
Important note: This tool provides general guidance. Always consult with a healthcare professional for proper diagnosis and treatment.
Quick Takeaways
- Angioedema can be driven by histamine or bradykinin pathways.
- Hereditary angioedema stems from a deficient C1 Esterase Inhibitor protein.
- ACE‑inhibitor drugs block bradykinin breakdown, often triggering attacks.
- Blood tests for C1 Esterase Inhibitor levels and complement activity help pinpoint the cause.
- Targeted treatments like icatibant or ecallantide can stop bradykinin‑mediated swelling fast.
Imagine swelling that shows up on your lips, eyes, or throat without a visible rash. It can feel like a sudden, unexplained emergency. That’s Angioedema - a rapid swelling of the deeper layers of skin and mucous membranes. Most people think it’s just a skin issue, but the real story runs deep into the immune system. Below you’ll learn how your body’s defense network can both cause and calm these episodes.
Angioedema is a localized, transient swelling that usually involves the lips, eyelids, tongue, and airway. It differs from hives because the skin’s surface looks normal - no raised welts, just a puffed‑up area.
Immune System is the collection of cells, proteins, and organs that protect you from infections and abnormal cells. It’s a fine‑tuned orchestra; when one player hits the wrong note, the whole performance can go off‑beat.
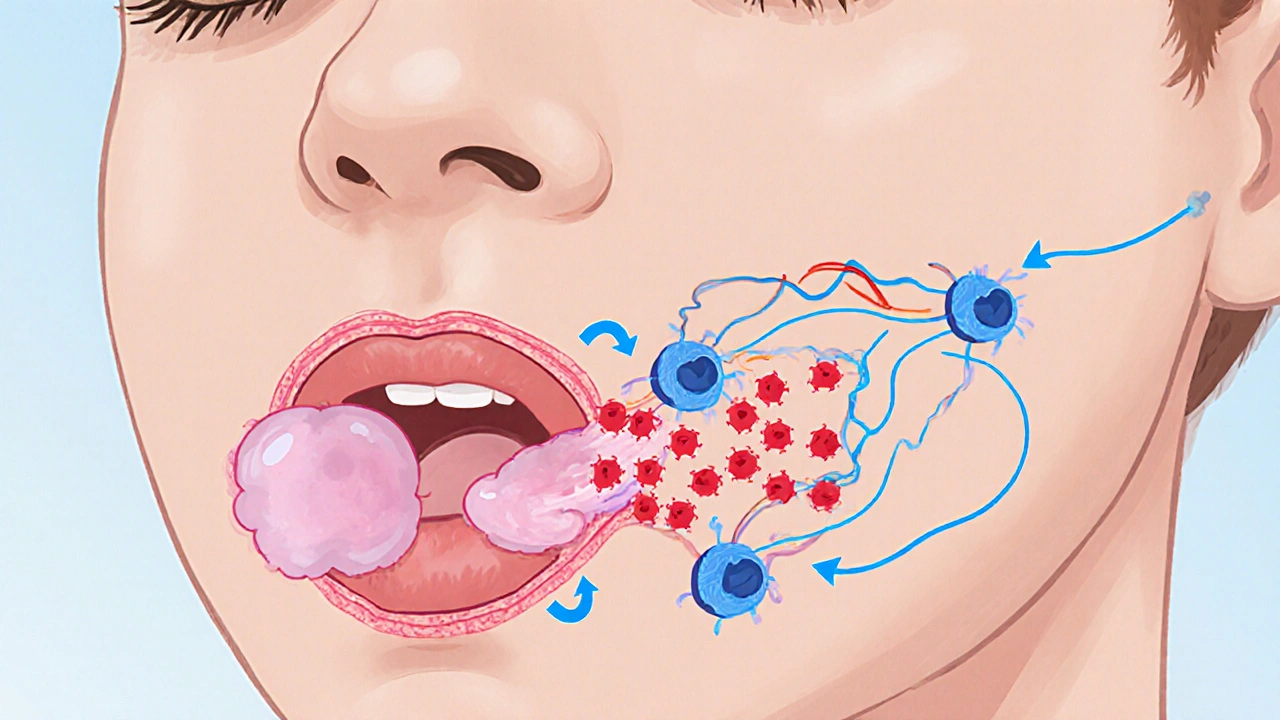
How the Immune System Normally Reacts
The immune system uses two main lines of defense. The first line is innate - quick, non‑specific responses like inflammation. The second line is adaptive - slower, highly specific attacks involving antibodies. Both lines release chemical messengers called mediators.
Two mediators matter most for angioedema: Histamine and Bradykinin. Histamine is released by Mast Cells during allergic reactions. Bradykinin, on the other hand, is a peptide that pops up when blood‑borne proteins like C1 Esterase Inhibitor are missing or when enzymes like ACE are blocked.
Types of Angioedema and Their Immune Links
Not all swelling follows the same rulebook. Clinicians group angioedema into three broad categories, each tied to a distinct immune pathway.
- Histamine‑mediated angioedema: triggers include foods, insect stings, or drugs that cause classic allergies. Mast cells release histamine, which makes blood vessels leaky.
- Bradykinin‑mediated angioedema: often genetic or drug‑induced. The culprit isn’t histamine, so antihistamines usually don’t help.
- Idiopathic or mixed: doctors can’t pinpoint a single mediator; sometimes both histamine and bradykinin play a role.
Understanding which pathway is active determines which treatment works.
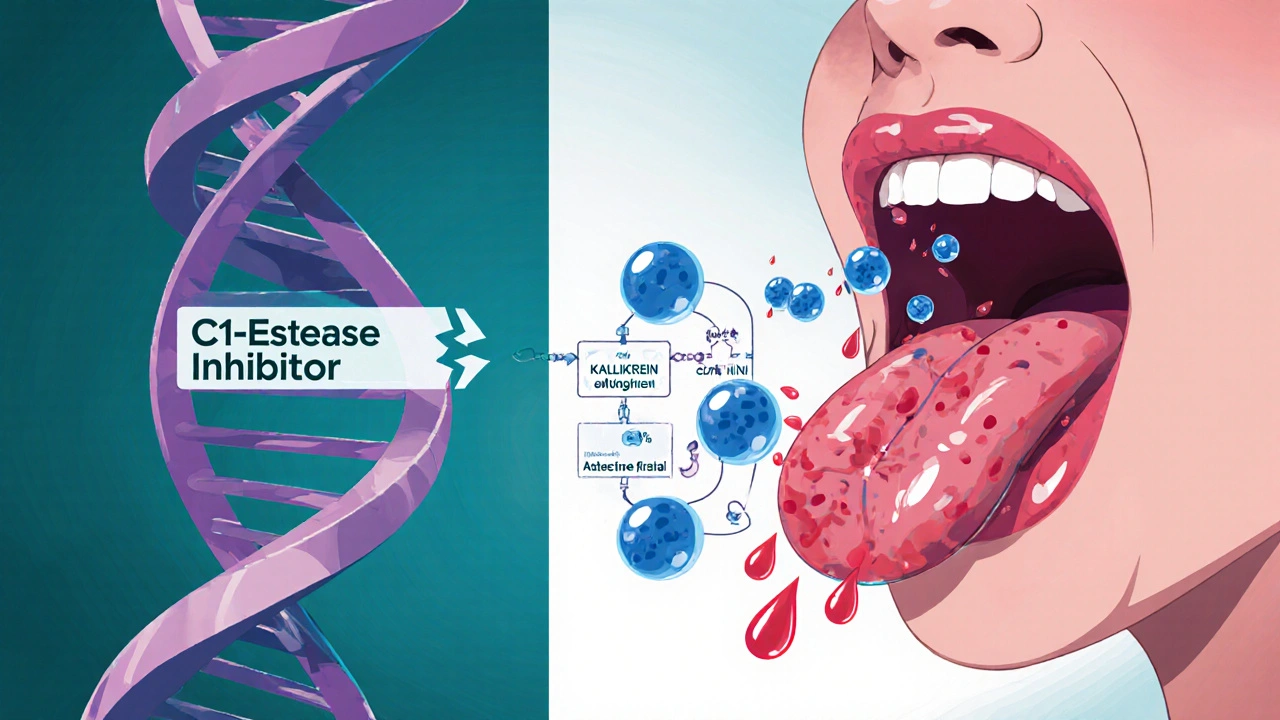
Hereditary Angioedema (HAE)
HAE is the textbook example of a bradykinin‑driven disorder. It’s passed down in families (autosomal dominant) and originates from a deficiency or dysfunction of C1 Esterase Inhibitor. Without enough of this protein, the complement system and kallikrein‑kinin cascade run amok, flooding the body with bradykinin.
Three subtypes exist:
- Type I - low levels of functional C1‑esterase inhibitor.
- Type II - normal levels but the protein doesn’t work properly.
- Type III - normal C1‑esterase inhibitor, usually linked to estrogen‑related triggers and seen mostly in women.
Blood tests that measure C1 Esterase Inhibitor concentration and activity, plus complement component C4 levels, confirm the diagnosis.
Acquired Angioedema (AAE)
AAE mimics HAE but isn’t inherited. It often pops up in older adults with autoimmune diseases (like lupus) or lymphoproliferative disorders. In these cases, the body produces antibodies that consume or block C1 Esterase Inhibitor, again leading to excess bradykinin.
Drug‑Induced Angioedema
The most common drug culprit is the class of blood‑pressure pills called ACE Inhibitors. ACE (angiotensin‑converting enzyme) normally breaks down bradykinin. Block the enzyme, and bradykinin lingers, causing swelling.
Other offending agents include:
- Direct renin inhibitors (e.g., aliskiren)
- Some non‑steroidal anti‑inflammatory drugs (NSAIDs) that can amplify mast‑cell degranulation
Diagnostic Toolbox
When a patient shows up with sudden swelling, doctors follow a step‑by‑step checklist:
- Take a detailed history - food, medication, family history, recent infections.
- Physical exam - look for urticaria, airway involvement, or signs of anaphylaxis.
- Lab work - C4 level, C1 Esterase Inhibitor antigenic level, functional assay, and sometimes tryptase (a mast‑cell marker).
- Genetic testing - for confirmed HAE subtypes, especially if family history is strong.
Imaging (e.g., ultrasound) can rule out deep‑tissue cellulitis when swelling is ambiguous.
Managing the Swell
The treatment toolbox is different for histamine‑ versus bradykinin‑driven attacks.
Histamine‑Mediated Approach
- Antihistamines (cetirizine, loratadine) - first line.
- Corticosteroids - for moderate to severe cases.
- Epinephrine auto‑injector - essential if airway is threatened.
Bradykinin‑Mediated Approach
- Icatibant - a bradykinin‑B2 receptor antagonist that stops swelling within 30 minutes.
- Ecallantide - a kallikrein inhibitor used for hereditary attacks.
- Plasma‑derived or recombinant C1 Esterase Inhibitor concentrate - replaces the missing protein in HAE/AAE.
- Fresh‑frozen plasma - a last‑ditch option when specific concentrates aren’t available.
Stopping an ACE‑inhibitor is the first step when drug‑induced angioedema is suspected; symptoms usually fade within 24‑48 hours.

Everyday Strategies to Reduce Risk
- Keep a medication list handy and share it with every new prescriber.
- Identify personal triggers - many HAE patients notice stress, dental work, or hormonal changes.
- Carry an emergency kit - antihistamine, icatibant (if prescribed), and a written action plan.
- Stay hydrated - dehydration can worsen bradykinin buildup.
- Consider prophylactic therapy - some patients use weekly C1 Esterase Inhibitor injections or oral berotralstat to cut the number of attacks.
When to Call for Help
If swelling involves the tongue, lips, or throat, or if breathing feels tight, treat it like an emergency. Even if you have a known diagnosis, the airway can close fast. Dial emergency services and use an auto‑injector if you have one.
Key Takeaways for Different Readers
Patients - Know whether your attacks are histamine or bradykinin driven; that determines which medication will help.
Family members - Learn the inheritance pattern of HAE and keep emergency contacts updated.
Healthcare providers - Use the diagnostic checklist, order complement labs early, and remember that stopping ACE‑inhibitors can be lifesaving.
| Feature | Histamine‑Mediated | Bradykinin‑Mediated (HAE/AAE/Drug) | Idiopathic/Mixed |
|---|---|---|---|
| Typical Triggers | Allergens, insect stings, NSAIDs | ACE‑inhibitors, C1‑esterase deficiency, auto‑antibodies | Often unknown |
| Key Mediator | Histamine | Bradykinin | Both or other peptides |
| Response to Antihistamines | Usually effective | Usually ineffective | Variable |
| Specific Therapies | Antihistamines, steroids, epinephrine | Icatibant, ecallantide, C1‑esterase replacement | Case‑by‑case |
| Lab Markers | Elevated tryptase (sometimes) | Low C4, low/ dysfunctional C1‑esterase inhibitor | Often normal |
Frequently Asked Questions
Can stress trigger angioedema?
Yes. Stress raises cortisol and can boost bradykinin levels in people with hereditary or acquired forms, leading to attacks.
Do antihistamines work for all types of angioedema?
Only for histamine‑mediated cases. Bradykinin‑driven attacks need drugs that block the bradykinin pathway.
Is hereditary angioedema curable?
There’s no cure, but prophylactic and on‑demand therapies can keep attacks rare and mild.
How fast does icatibant work?
Patients often notice relief within 30-60 minutes after a subcutaneous injection.
Should I stop ACE‑inhibitors if I’ve had swelling?
Yes. Discontinue the drug and talk to your doctor about alternative blood‑pressure meds. Swelling usually resolves in 1-2 days.
By connecting the dots between mediators, genetics, and medications, you can turn a scary swelling episode into a manageable health event. Keep the checklist handy, know your trigger, and don’t hesitate to call emergency services if the airway looks threatened.

Tom Green
October 16, 2025 AT 19:22If you suspect bradykinin‑mediated angioedema, get C4 and C1‑INH labs ASAP.
Emily Rankin
October 17, 2025 AT 18:58The cascade of stress hormones can tip the delicate balance between histamine and bradykinin, turning a harmless trigger into a full‑blown angioedema episode. When cortisol spikes, it can modulate mast cell stability, making them more prone to degranulation even in the absence of classic allergens. Simultaneously, the kallikrein‑kinin system becomes more active, producing excess bradykinin that leaks into the submucosal layers. For patients with hereditary angioedema, this double whammy explains why a bad day at work can precipitate an attack that feels like a ticking time bomb. The literature shows that low C4 levels are a reliable sentinel of an underlying complement deficiency, so ordering that panel early can save crucial minutes. Moreover, measuring functional C1‑esterase inhibitor activity distinguishes between type I and type II HAE, guiding whether replacement therapy or a kallikrein inhibitor is appropriate. In the emergency setting, an icatibant injection can restore airway patency within thirty minutes, essentially buying time for definitive care. Yet many clinicians still reach for antihistamines first, a habit that delays effective treatment when bradykinin is the culprit. Education of primary care physicians about the distinct pathways is as important as the drugs themselves. Patients should also keep a written action plan, because in the chaos of swelling the mind can’t process complex dosing schedules. Hydration plays a surprisingly big role; dehydration concentrates plasma proteins and can amplify bradykinin signaling. Lifestyle modifications, like avoiding trigger foods and managing stress with mindfulness, complement pharmacologic prophylaxis. For those on ACE inhibitors, a simple medication review often uncovers the root cause, allowing a switch to an ARB without losing blood pressure control. The emerging oral agents, such as berotralstat, offer a convenient prophylactic option that can reduce attack frequency dramatically. Ultimately, understanding the immunologic choreography empowers patients and providers alike to turn a frightening swelling event into a manageable one. So remember: the key is to match the mediator with the medicine, not to guess and hope.
Rebecca Mitchell
October 18, 2025 AT 18:35yeah you gotta get those labs done quick cuz waiting can make things worse its not just a formality you need real results fast you know the thing about C1 inhibitor deficiency is that it shows up in a lot of people without warning so testing early can literally save a life dont skip it
Roberta Makaravage
October 19, 2025 AT 18:12Everyone should know that bradykinin does NOT respond to antihistamines 🙅♀️💊 The only way to stop a bradykinin‑driven episode is to block its pathway directly, either with icatibant or a C1‑esterase inhibitor replacement. Ignoring this fact leads to unnecessary suffering and wasted emergency visits. 📢
Russell Abelido
October 20, 2025 AT 17:48Exactly, the urgency can’t be overstated – when a patient’s tongue starts swelling, every minute counts. :) Having an emergency kit at hand, including a subcutaneous icatibant dose, makes the difference between a scary night and a calm one.
Steve Holmes
October 21, 2025 AT 17:25Thanks for the insight! It’s awesome to see a clear breakdown of when antihistamines work and when they don’t. I’ll make sure to share this with my clinic buddies, especially the part about ordering C4 and C1‑INH labs early. 👍
Chris Beck
October 22, 2025 AT 17:02Look folks, this is simple. If you see swelling and no rash, think bradykinin. Get labs. Do not waste time on steroids. Use the right drug. Period!!
Sara Werb
October 23, 2025 AT 16:38Wow, this whole thing is a huge CONSPIRACY! The pharma guys never tell u that ACE inhibitors are a trap!! They want u sWallow in chronic swelling for profit!!!
Winston Bar
October 24, 2025 AT 16:15Yeah right, like anyone believes that. I think it’s all just hype; most people never even get a real attack. The whole “danger” is overblown.
Lauren Sproule
October 25, 2025 AT 15:52Hey everyone, just wanted to add that keeping a simple checklist on your fridge can really help during an emergency. It’s all about staying calm and having the right meds ready.
CHIRAG AGARWAL
October 26, 2025 AT 14:28Checklists are fine but they’re just another thing to remember. People forget them anyway. Maybe just trust your doctor’s advice instead.
genevieve gaudet
October 27, 2025 AT 14:05From a cultural perspective, many societies view sudden swelling as a spiritual warning rather than a medical issue. Integrating traditional beliefs with modern diagnostics can improve patient compliance and outcomes.
Patricia Echegaray
October 28, 2025 AT 13:42Sure, but don’t forget that the “big pharma” agenda is behind every new drug. They push expensive icatibant while ignoring cheaper natural alternatives that could work if people just looked deeper.
Kevin Adams
October 29, 2025 AT 13:18Drama alert – the battlefield inside our bodies is epic! Histamine vs. bradykinin, each fighting for control of our faces. Who will win? The answer lies in the labs, my friends.
Katie Henry
October 30, 2025 AT 12:55In pursuit of excellence, it is imperative that clinicians adhere to evidence‑based protocols, promptly differentiate between histamine‑ and bradykinin‑mediated angioedema, and administer the appropriate therapeutic agent without delay.
Joanna Mensch
October 31, 2025 AT 12:32The truth is hidden; the immune system is being monitored by unseen forces.