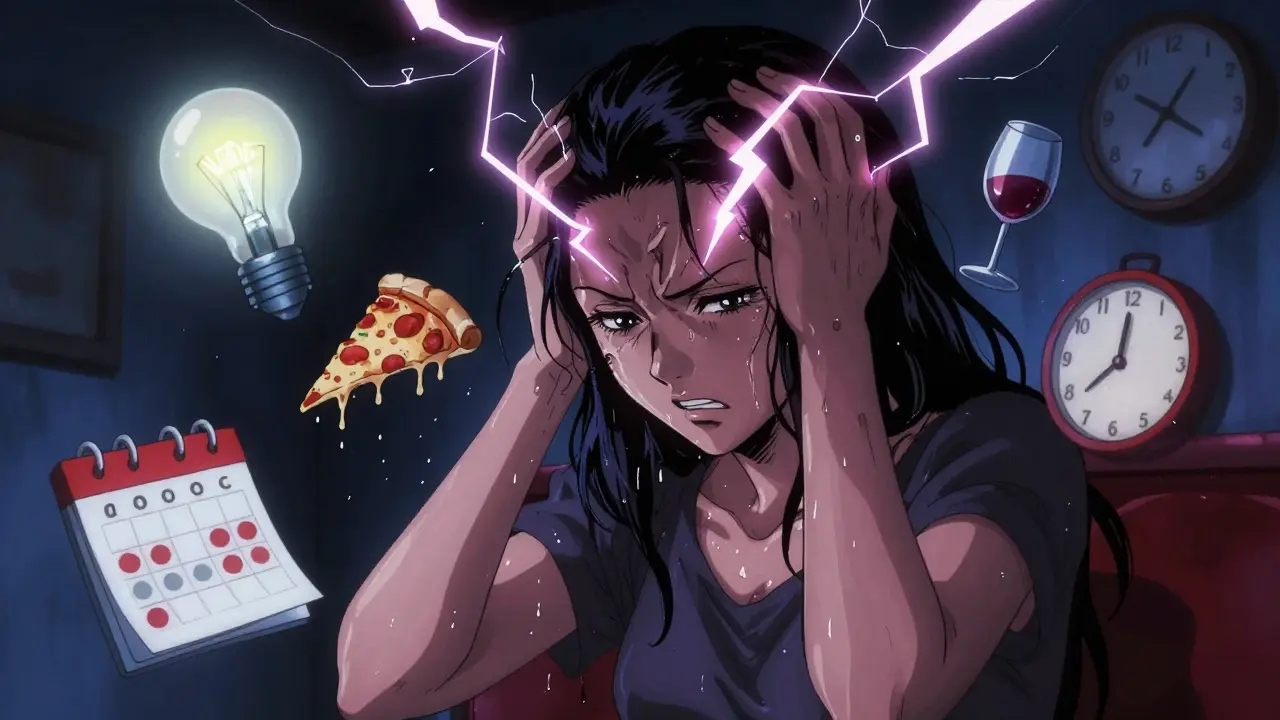
Migraine isn't just a bad headache. It’s a neurological event that can knock you out for hours-or days. You might feel nauseous, blind from light, deaf from sound, or stuck in a fog of pain that doesn’t respond to ordinary painkillers. If you’ve had one, you know: this isn’t something you can just push through.
Half of all migraine attacks happen between 4 a.m. and 9 a.m. That’s not random. It’s your body’s rhythm, your sleep cycle, your stress levels-all lining up to trigger a storm in your brain. And while everyone’s migraine looks different, the triggers, treatments, and tools to manage them are surprisingly consistent-if you know where to look.
What Actually Triggers a Migraine?
There’s no single cause of migraine. Instead, your brain has a threshold. When too many triggers pile up, you cross it-and the attack starts. One stressor alone might not do it. But stress + skipped lunch + bright lights + poor sleep? That’s the combo that hits.
Stress is the biggest trigger. About 70% of people with migraines say stress sets off their attacks. But here’s the twist: it’s not always during the stress. Many get what’s called a “let-down migraine”-right after a big deadline, a busy week, or a vacation ends. Your body relaxes, your cortisol drops, and boom. The headache hits.
Sleep patterns matter just as much. Too little? Too much? Irregular bedtimes? All of them can spark an attack. People who work night shifts or travel across time zones often see their migraines flare. If you’re sleeping in on weekends, that’s not a treat-it’s a risk.
Hormones play a major role, especially for women. Around 65% of female migraine sufferers report attacks tied to their cycle-right before or during menstruation. Pregnancy can help some, but others get worse. Birth control pills? They can help or hurt, depending on the type and your body’s response.
Dietary triggers are tricky. Not everyone reacts the same. But the usual suspects show up again and again: alcohol (especially red wine), aged cheeses, processed meats with nitrates, MSG, artificial sweeteners like aspartame, and chocolate. Caffeine? It’s a double-edged sword. A cup of coffee can stop a migraine in its tracks-for some. For others, skipping caffeine triggers a headache. Too much, and it becomes the problem.
Weather changes are real. A drop in barometric pressure before a storm, sudden humidity, high altitude during flights-these can all flip the switch. Lightning? Studies show it can increase migraine risk by 30% in sensitive people.
And then there’s the senses. Bright or flickering lights-fluorescent bulbs, phone screens, sunlight on snow-can be brutal. Loud, repetitive noises. Strong smells-perfume, cigarette smoke, even fresh paint. One person’s pleasant scent is another’s migraine starter.
How to Find Your Personal Triggers
Not everyone reacts to the same things. That’s why tracking is non-negotiable. You need a migraine diary. Not a fancy app-just a notebook or a simple phone note. Write down:
- When the headache started and how long it lasted
- What you ate or drank in the 24 hours before
- Your sleep hours and bedtime routine
- Your stress level (1 to 10)
- Weather changes or travel
- Any strong smells, lights, or noises
- Medications taken, including caffeine
Do this for at least two months. Look for patterns. Do you always get a migraine after eating pizza? After sleeping past 10 a.m.? After a long meeting on a Friday? That’s your data. That’s your power.
Don’t assume you know your triggers. One person thinks chocolate is the culprit-until they realize it was the red wine they had with it. Or they blame stress, but it’s actually the combination of stress and skipping meals. Your diary helps you see the real combo.
Preventive Medications: What Actually Works
If you’re having more than four migraine days a month, or if your attacks are disabling, preventive medication is worth considering. These aren’t painkillers. They’re taken daily to reduce how often and how badly migraines hit.
The most common preventive drugs include:
- Beta-blockers like propranolol and timolol-originally for blood pressure, they help calm overactive nerves in the brain.
- Anticonvulsants like topiramate and valproate-these stabilize electrical activity in the brain and can reduce attack frequency by half in many people.
- Tricyclic antidepressants like amitriptyline-even if you’re not depressed, these help regulate pain signals and improve sleep, which cuts down attacks.
- CGRP inhibitors like erenumab and fremanezumab-these are newer, injectable drugs that block a protein linked to migraine pain. They’re expensive, but for some, they’re life-changing. Many users report cutting their migraine days by 50% or more.
These aren’t quick fixes. It can take 2-3 months to see results. And side effects happen-fatigue, tingling, weight changes, brain fog. But if you’ve tried lifestyle changes and still get knocked out weekly, these drugs can give you your life back.
Not everyone needs them. Some people manage with triggers alone. Others need a mix. Your doctor will help you pick based on your health history, other conditions, and what you can tolerate.
Acute Care: What to Take When the Pain Hits
When a migraine is already here, you need fast relief. The goal isn’t to cure it-it’s to stop it from getting worse and bring you back to normal as quickly as possible.
First-line options:
- NSAIDs like ibuprofen or naproxen-effective for mild to moderate attacks. Take them early, before the pain peaks.
- Triptans like sumatriptan or rizatriptan-these are migraine-specific. They narrow blood vessels and block pain pathways. They work for about 70% of people. Available as pills, nasal sprays, or injections.
- Gepants like ubrogepant and rimegepant-newer oral drugs that block CGRP without narrowing blood vessels. Great for people who can’t take triptans due to heart issues.
- Anti-nausea meds like metoclopramide or prochlorperazine-often given with pain meds because nausea makes everything worse.
Caffeine? Yes, sometimes. A small dose (like in Excedrin Migraine) can boost the effect of painkillers. But don’t use it daily-it can lead to rebound headaches.
Timing matters. Take your acute meds as soon as you feel the warning signs-not when the pain is at 10/10. The earlier, the better.
Don’t overuse. Taking painkillers more than 10 days a month can turn your migraines into chronic daily headaches. That’s called medication-overuse headache. It’s real. It’s common. And it’s fixable-if you stop the overuse and work with your doctor.
What Doesn’t Work (and Why)
There’s a lot of noise out there. Essential oils? Maybe soothing, but no strong evidence they stop migraines. Chiropractic neck adjustments? Can help with tension headaches, but not necessarily migraines. CBD? Some small studies show promise, but it’s not yet proven.
And don’t fall for “miracle diets.” Cutting out every trigger food might help-but if you’re not tracking, you’re guessing. Starving yourself won’t prevent migraines. It’ll make them worse.
Stress management isn’t just yoga. It’s consistency. Regular meals. Fixed sleep. Not letting your life spiral into chaos. That’s the real prevention.

When to See a Doctor
You don’t need to suffer in silence. See a neurologist or headache specialist if:
- Your migraines are getting worse or more frequent
- Over-the-counter meds don’t help anymore
- You have new symptoms like vision loss, weakness, or confusion
- You’re using painkillers more than 10 days a month
- Your attacks are disrupting work, family, or daily life
Migraine is treatable. It’s not a sign of weakness. It’s a medical condition with real biology behind it. And with the right plan-trigger tracking, preventive meds if needed, and timely acute treatment-you can take back control.
Living With Migraine: The Real Strategy
The goal isn’t to never have another migraine. The goal is to reduce them enough that they don’t rule your life.
Start with your diary. Find your triggers. Then build a routine around them: sleep at the same time, eat regularly, manage stress with movement-not just meditation, but walking, swimming, anything that moves your body.
Don’t wait until you’re in pain to act. Prevention is quieter than treatment. It’s not glamorous. But it works.
And if meds are part of your plan? That’s not failure. That’s strategy. Millions of people take daily pills for blood pressure, thyroid, or cholesterol. Migraine meds are no different. They’re tools. Use them.
You’re not broken. You’re not imagining it. You just need the right system-and you already have the first step: you’re looking for answers. That’s how it starts.

Hadi Santoso
December 16, 2025 AT 07:58Man, I thought I was just bad at sleeping until I started tracking my migraines. Turns out, sleeping in on weekends is my personal enemy. Now I set an alarm even on Sundays. No more ‘let-down’ headaches. Life’s weird like that.