High blood pressure doesn’t come with warning signs. You might feel fine, but over time, it silently damages your heart, kidneys, and arteries. That’s why millions of people take blood pressure medications every day-not because they’re sick, but because they want to stay that way. The most common drugs? ACE inhibitors, beta blockers, calcium channel blockers, diuretics, and ARBs. But which one is right for you? And why do some people switch meds after just a few weeks?
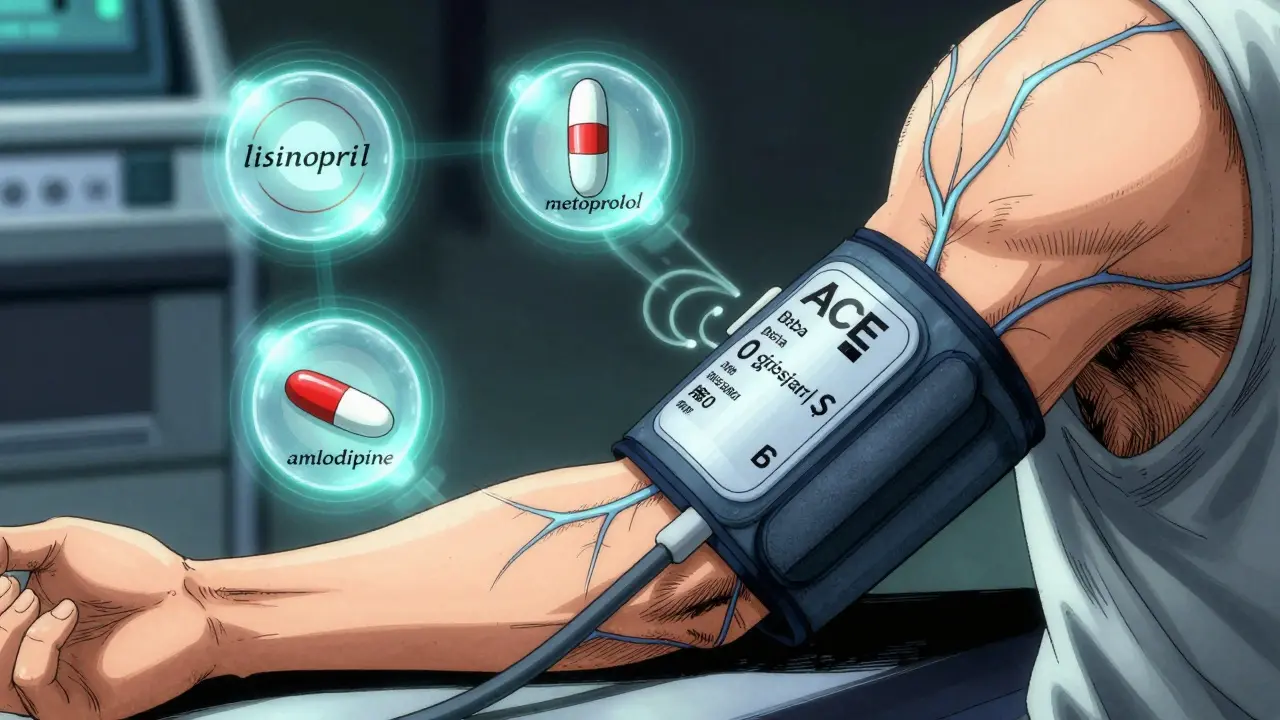
What ACE Inhibitors Do (and Why People Stop Taking Them)
ACE inhibitors, like lisinopril and enalapril, are among the most prescribed blood pressure drugs in the U.S. Their name comes from how they work: they block the enzyme that turns angiotensin I into angiotensin II, a chemical that tightens blood vessels. Less angiotensin II means relaxed arteries and lower pressure. These drugs are especially helpful if you have diabetes, kidney disease, or heart failure. But here’s the catch: about 1 in 5 people develop a dry, hacking cough. It’s not dangerous, but it’s relentless. One user on Reddit said they’d been on lisinopril for eight months-night after night, coughing so hard they couldn’t sleep. Switching to losartan (an ARB) stopped it within three days. That cough isn’t rare. Drugs.com reviews show 29% of people on ACE inhibitors report it. It’s why so many end up switching to ARBs like valsartan or losartan, which block the same pathway but don’t trigger the cough. For many, that’s the only difference they notice-same blood pressure control, no sleepless nights.Beta Blockers: Slowing the Heart, Sometimes Too Much
Beta blockers like metoprolol and atenolol don’t relax blood vessels. Instead, they slow your heart rate and reduce how hard your heart pumps. That lowers pressure, yes-but it also drains energy. People on beta blockers often report feeling tired, sluggish, or even depressed. A Drugs.com review from June 2023 called metoprolol "the worst medication I’ve ever taken"-said it left them too exhausted to work. Others notice sexual side effects or cold hands and feet. That’s why they’re not first-line anymore for most people. The ASCOT trial back in 2005 showed amlodipine (a calcium channel blocker) was better than atenolol at preventing heart attacks and strokes. Today, beta blockers are mostly used if you’ve had a heart attack, have heart failure, or have a fast or irregular heartbeat. If you’re just starting out with high blood pressure, your doctor is more likely to pick something else.Calcium Channel Blockers: The Go-To for Most People
If you’re looking for the most reliable, well-tolerated option, amlodipine is it. It’s a calcium channel blocker-specifically, a dihydropyridine-that opens up arteries by blocking calcium from entering muscle cells in your blood vessel walls. It’s cheap, effective, and works regardless of your weight. Unlike hydrochlorothiazide (a diuretic), which loses effectiveness in leaner people, amlodipine works just as well whether you’re overweight or not. Studies show it cuts stroke risk better than ACE inhibitors. Side effects? Swelling in the ankles is common-nearly 40% of users report it. Headaches and flushing happen too. But these usually fade after a few weeks. And unlike ACE inhibitors, there’s no cough. No fatigue like beta blockers. That’s why it’s one of the top two most prescribed blood pressure drugs in the U.S., behind only lisinopril.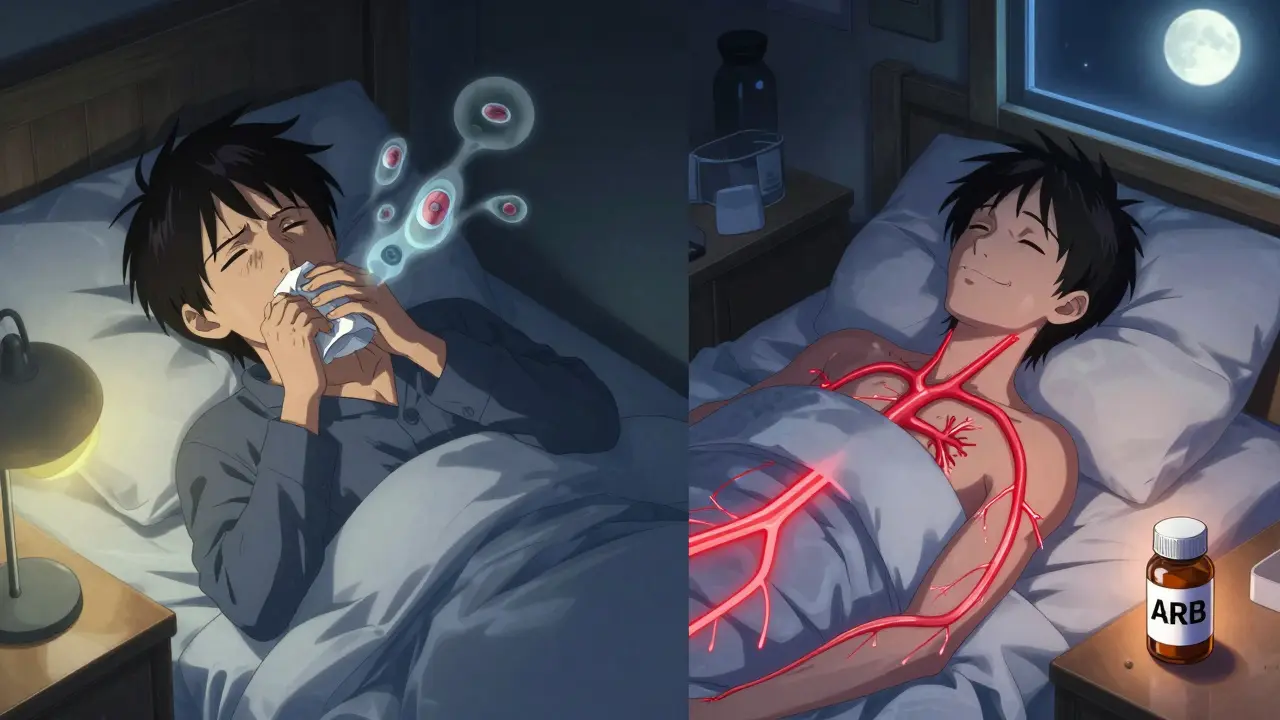
Diuretics: The Old Workhorse Still Winning
Diuretics, often called "water pills," help your kidneys flush out extra salt and water. Less fluid in your blood means lower pressure. The most common are thiazide diuretics like hydrochlorothiazide and chlorthalidone. Here’s something most people don’t know: chlorthalidone is better than hydrochlorothiazide. It lasts longer, controls blood pressure 24 hours, and reduces heart attacks and strokes more effectively. A 2020 trial found chlorthalidone cut cardiovascular events by 21% more than hydrochlorothiazide. Yet most doctors still prescribe hydrochlorothiazide because it’s been around longer and is more familiar. Side effects? Frequent urination (42% of users), dizziness, and low potassium. That’s why your doctor will check your electrolytes every few months. If you’re on a diuretic, you might need a potassium supplement or a potassium-sparing pill like amiloride.Why Combination Pills Are Becoming the Norm
Most people don’t get their blood pressure under control with just one pill. The American Heart Association says nearly half of hypertensive patients need two or more drugs. That’s why fixed-dose combinations are everywhere now. Examples:- Exforge = amlodipine + valsartan
- Lotrel = amlodipine + benazepril (an ACE inhibitor)
- Diovan HCT = valsartan + hydrochlorothiazide
What Your Doctor Won’t Always Tell You
There are big differences in how these drugs work for different people. For example:- Black patients often respond better to calcium channel blockers or diuretics than to ACE inhibitors or ARBs-unless they have kidney disease.
- Older adults (60+) with isolated high systolic pressure (top number) do best with calcium channel blockers.
- If you have diabetes or kidney disease, ACE inhibitors or ARBs are usually preferred because they protect your kidneys.
- If you have asthma, avoid beta blockers-they can trigger attacks.
- If you have diabetes, beta blockers can hide signs of low blood sugar, like a fast heartbeat.

Cost Matters More Than You Think
Most of these drugs are generic. That means they’re cheap.- Lisinopril: $4-$8/month
- Amlodipine: $5-$10/month
- Hydrochlorothiazide: $3-$7/month
- Losartan: $6-$12/month
What Happens When Nothing Seems to Work?
If you’re on three or more meds and your blood pressure still won’t budge, you might have resistant hypertension. That’s when your doctor might consider spironolactone-a low-dose mineralocorticoid blocker. It’s not a first-line drug, but for stubborn cases, it’s one of the most effective add-ons. There’s also a new option: renal denervation. In November 2023, the FDA approved the first implantable device that uses radio waves to calm overactive nerves around the kidneys. Early results show it lowers blood pressure by 8-9 mmHg more than a placebo. It’s not for everyone-but it’s a real breakthrough for people who’ve tried everything else.What You Should Do Next
If you’re on blood pressure medication:- Take it at the same time every day-even if you feel fine.
- Don’t stop because of side effects. Talk to your doctor first.
- Get your blood pressure checked regularly at home. Don’t rely only on clinic visits.
- Ask if you’re on chlorthalidone or hydrochlorothiazide. If it’s the latter, ask if switching would help.
- If you have a dry cough, ask about switching to an ARB.
- If you’re tired all the time, ask if beta blockers could be the cause.
Can I stop taking blood pressure medication if my numbers are normal?
No-not without talking to your doctor. Normal blood pressure on meds means the medication is working, not that you’re cured. Stopping suddenly can cause your pressure to spike back up, sometimes dangerously. Some people can reduce or stop meds after losing weight or making big lifestyle changes, but only under medical supervision.
Which blood pressure medicine has the least side effects?
Amlodipine (a calcium channel blocker) generally has the best balance of effectiveness and tolerability. It doesn’t cause cough, fatigue, or sexual side effects like other classes. The most common issue is ankle swelling, which often fades after a few weeks. Diuretics like chlorthalidone are also well-tolerated long-term but require electrolyte monitoring.
Why do some people need two or three blood pressure pills?
High blood pressure has multiple causes-tight arteries, excess fluid, overactive nerves. One drug usually only targets one mechanism. Combining two or three drugs that work in different ways gives you better control than doubling one drug’s dose. Plus, lower doses of multiple drugs mean fewer side effects.
Are natural remedies enough to replace blood pressure meds?
No-not if your blood pressure is consistently above 140/90. Lifestyle changes like reducing salt, losing weight, and exercising help, and they should always be part of your plan. But for most people with stage 1 or 2 hypertension, medication is necessary to reduce the risk of stroke, heart attack, or kidney damage. Don’t replace meds with supplements unless your doctor agrees.
How long does it take for blood pressure meds to work?
You might see a drop in a few days, but full effect usually takes 2 to 6 weeks. Some drugs, like amlodipine, build up slowly in your system. Your doctor will likely check your blood pressure every 2 to 4 weeks until it’s stable. Don’t rush to change meds if you don’t see results right away.

Shae Chapman
December 30, 2025 AT 10:35This post is 🔥 seriously one of the clearest breakdowns of BP meds I’ve ever read. I was on lisinopril for a year and thought I was just getting old-turns out it was the cough killing my sleep. Switched to losartan and it’s like I got my life back. No more 3 a.m. hacking marathons. 🙌
kelly tracy
December 31, 2025 AT 05:48Of course the only person who actually read this is the one who got lucky with amlodipine. Most of us are stuck on hydrochlorothiazide because our insurance won’t cover chlorthalidone even though it’s better. And don’t even get me started on how doctors ignore the fact that women metabolize these drugs differently.
srishti Jain
January 2, 2026 AT 04:22amlodipine = ankle swelling. no one talks about that. i stopped because my feet looked like balloons. then i got on spironolactone and now i pee all day. no win.
Glendon Cone
January 2, 2026 AT 07:35Big shoutout to the author for including the grapefruit warning-that’s something even some docs forget. I was on felodipine and drank my morning OJ like a champ until my BP spiked. Now I know. Also, if you’re tired on beta blockers? It’s not ‘just aging.’ Talk to your doc. You deserve to feel human.
henry mateo
January 3, 2026 AT 01:44thx for this i read it all. i was on metoprolol and felt like a zombie. switched to amlodipine and now i can play with my kids without napping after dinner. still got the swollen ankles but hey at least i’m not dead inside 😅
Nadia Spira
January 3, 2026 AT 17:36Let’s be real-this is just pharma’s PR pamphlet dressed as medical advice. ACE inhibitors cause cough? Shocking. Beta blockers cause fatigue? Groundbreaking. The real issue is that we’ve turned chronic physiological regulation into a pill-pushing carnival. The body isn’t a machine to be hacked with pharmacological bandaids. Lifestyle? Sure. But this whole system is designed to keep you medicated, not healed. The fact that you’re reading this means you’re already part of the problem.
Colin L
January 5, 2026 AT 08:21I’ve been on three different regimens over the past seven years and I can tell you this: the only thing that’s consistent is how little doctors actually listen. I told my cardiologist I was getting dizzy on chlorthalidone-he said ‘it’s just water loss, drink more.’ I lost 12 pounds in two weeks and ended up in the ER. They finally switched me to a combo pill and now I’m stable. But if I hadn’t pushed? I’d be dead. Why is patient advocacy the only thing that saves you in this system?
Hayley Ash
January 5, 2026 AT 23:50So amlodipine is the ‘best’ because it doesn’t make you cough or feel like a sloth? Cool. Meanwhile my grandma’s on it and her ankles are bigger than my head. And you call that a win? Also-why does everyone act like chlorthalidone is some secret miracle drug? It’s been around since 1957. Doctors just don’t read journals anymore. They read drug reps’ PowerPoints.
Kelly Gerrard
January 7, 2026 AT 21:29Thank you for this comprehensive guide. It is imperative that patients understand that hypertension is a lifelong condition requiring consistent management. Medication adherence saves lives. Do not discontinue therapy without professional oversight. Your health is your greatest asset.
Cheyenne Sims
January 8, 2026 AT 16:59As a board-certified physician, I must correct a critical misstatement: ARBs do not ‘block the same pathway’ as ACE inhibitors-they block the receptor, not the enzyme. This distinction matters clinically. Also, the claim that ‘amlodipine works regardless of weight’ is misleading. While it’s more predictable than thiazides, pharmacokinetics still vary by BMI, renal function, and CYP3A4 activity. Please cite primary literature before making broad generalizations.
Sandeep Mishra
January 8, 2026 AT 20:49For anyone feeling overwhelmed-this isn’t about finding the ‘perfect’ pill. It’s about finding the one that lets you live. I’ve been on lisinopril, then amlodipine, then a combo. Each time, I adjusted. My BP is stable. I hike, I cook, I laugh. The meds aren’t the enemy. The silence around side effects is. Keep talking. Keep asking. You’re not alone.
Aayush Khandelwal
January 10, 2026 AT 03:15Here’s the real tea: BP meds are like socks. You try a few pairs until one doesn’t give you blisters. Amlodipine? That’s the cashmere pair. Losartan? The comfy cotton. Metoprolol? The wool ones that itch like hell. And yeah, sometimes you gotta wear two pairs-because one just ain’t enough. The system’s messy, but your health ain’t negotiable.
Henry Ward
January 10, 2026 AT 17:12Why do people still take these drugs? Why not just eat better? Why not fast? Why not meditate? It’s not rocket science. You want to fix your blood pressure? Stop being lazy. Stop eating processed junk. Stop drinking soda. Stop being a zombie in front of a screen. Medication is a crutch for people who refuse to take responsibility. This whole article is enabling.
Kunal Karakoti
January 12, 2026 AT 11:14What if the real question isn’t which drug works best-but why we’ve built a system where 70% of adults need pills just to stay alive? We treat symptoms like crimes instead of signals. Maybe we should be asking: why are our cities designed without sidewalks? Why is fresh food a luxury? Why does healthcare profit from sickness? The pill is a bandage. The wound is society.