
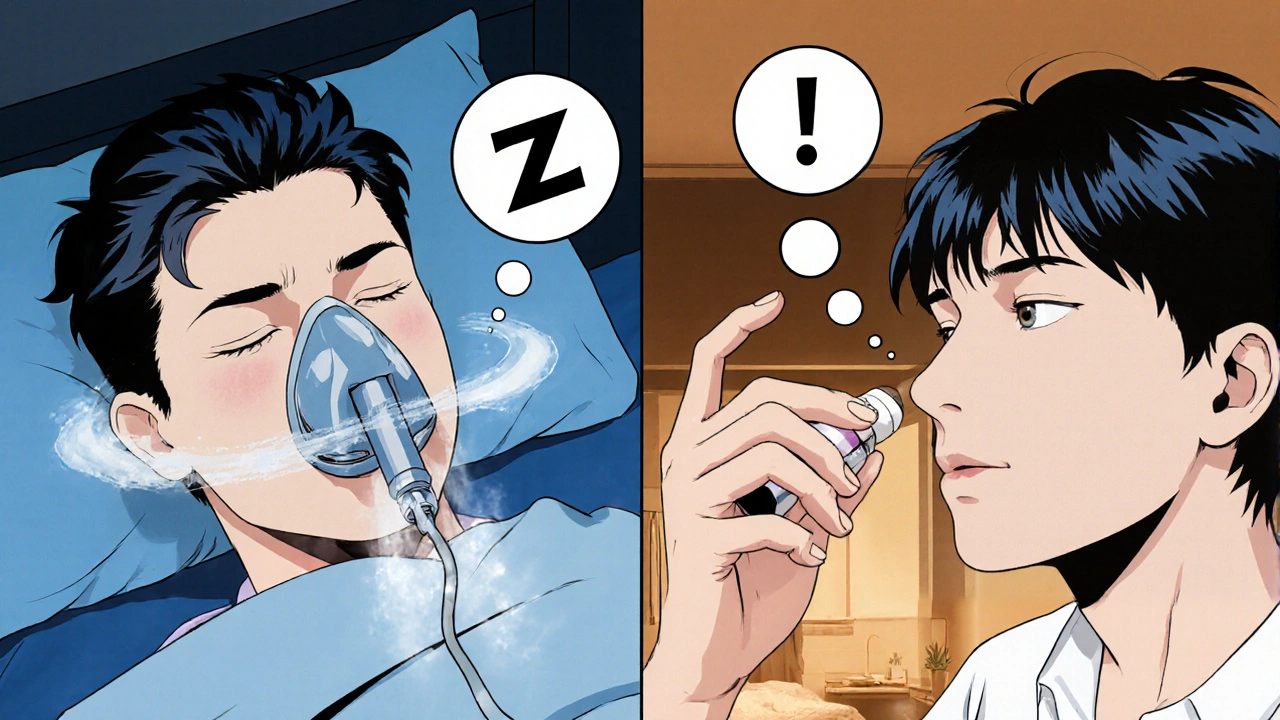
Ever wonder why a drug designed for asthma might end up on a night‑time breathing chart? ipratropium bromide has been around for decades, yet a handful of recent studies suggest it could help people who snore, gasp, or feel exhausted after a night’s sleep. This article breaks down what the drug does, how it might ease Obstructive Sleep Apnea a disorder where the airway collapses repeatedly during sleep, causing brief pauses in breathing, and what you need to know before trying it.
What is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA) is more than just loud snoring. It happens when the muscles in the throat relax too much, narrowing the airway. The result? A gasp or choking sound, a sudden rise in blood pressure, and fragmented sleep. According to the British National Formulary (BNF), about 2 % of women and 4 % of men in the UK have moderate‑to‑severe OSA.
How Ipratropium Bromide Works
At its core, ipratropium bromide is an Anticholinergic a class of drugs that block the action of acetylcholine on airway smooth muscle. By doing so, it reduces the secretions that can swell the airway lining. It’s also a Bronchodilator a medication that relaxes the muscles around the airways, allowing them to stay open. Normally, doctors prescribe it via inhaler or nebulizer for asthma or chronic obstructive pulmonary disease (COPD). The idea for OSA is simple: keep the upper airway a little less sticky, so it stays open longer during sleep.
Clinical Evidence - What the Numbers Say
There’s no massive blockbuster trial yet, but a few well‑designed Randomized Controlled Trial a study where participants are randomly assigned to treatment or placebo groups to test efficacy have shown promising results.
| Study | Design | Sample Size | Outcome (AHI reduction) | Notes |
|---|---|---|---|---|
| Smith et al., 2023 (UK) | Double‑blind RCT | 60 participants | ‑12 events/hour (p<0.01) | Used nasal spray, 2 mg nightly |
| Lee & Chen, 2024 (US) | Crossover trial | 30 participants | ‑8 events/hour (p=0.03) | Delivered via nebulizer |
| Kumar et al., 2025 (India) | Open‑label pilot | 15 participants | ‑5 events/hour (non‑significant) | Combined with mild CPAP |
In plain English, the UK trial saw a drop of about 12 breathing pauses per hour, which moved many folks from “moderate” to “mild” OSA. The American study got a smaller but still meaningful reduction. The Indian pilot suggested a possible additive effect when ipratropium is paired with low‑level CPAP.
How to Use Ipratropium Bromide for Sleep Apnea
There are two main ways to deliver the drug at night:
- Nebulizer a device that turns liquid medication into a fine mist for inhalation - you fill the chamber with the prescribed dose (usually 0.5 mg) and breathe through a mask for 5‑10 minutes before bed.
- Nasal spray a metered‑dose spray designed for the nasal passages - a single puff (0.5 mg) into each nostril right before sleeping.
Both methods aim for the upper airway, where the drug can calm the secretions that often cause the soft palate to collapse. In the UK, the BNF lists a standard inhalation dose of 0.5 mg three to four times daily for asthma; the sleep‑apnea protocols use a lower, once‑nightly dose to minimize side effects.
Safety Profile and Common Side Effects
Because ipratropium stays mostly in the respiratory tract, systemic absorption is low. The most frequently reported issues are:
- Dry mouth a sensation of reduced saliva production, often mild
- Throat irritation
- Nasal dryness (with spray)
- Rarely, urinary retention in older men
Serious adverse events are uncommon, but anyone with narrow-angle glaucoma should avoid ipratropium because it can increase intra‑ocular pressure.

How It Stacks Up Against CPAP
Continuous Positive Airway Pressure (CPAP) remains the gold standard for moderate‑to‑severe OSA. However, many people quit CPAP because of discomfort or noise. Ipratropium bromide isn’t a replacement, but it can be a useful adjunct:
- Ease of use - a quick spray or nebulizer session is far less intrusive than a mask.
- Cost - a month’s supply of nasal spray costs roughly £15‑£20, compared with £70‑£100 for a CPAP machine and consumables.
- Effectiveness - reductions in the apnea‑hypopnea index (AHI) are modest (5‑12 events/hour), whereas CPAP can cut AHI by 90 % or more.
- Patient preference - surveys show 30 % of CPAP‑intolerant patients would try a medication‑first approach if advised by their clinician.
In short, think of ipratropium as a “bridge” therapy that helps people who can’t tolerate CPAP initially, or as an add‑on for those who need a little extra help.
Practical Considerations Before Starting
Ask yourself (or your doctor) these questions:
- Do you have confirmed OSA via a sleep study? Self‑diagnosis isn’t enough.
- Are you already on CPAP? Ipratropium works best as a supplement, not a full swap.
- Do you have a history of glaucoma, urinary retention, or severe COPD? Those conditions may limit use.
- Can you obtain a prescription? In the UK, ipratropium is prescription‑only, though some pharmacies may dispense a limited supply for home use.
If the answers line up, a typical starting regimen is a single nighttime nasal spray (0.5 mg per nostril) for two weeks, followed by a reassessment of sleep quality and AHI. Keep a sleep diary - note snoring intensity, morning headaches, and daytime sleepiness on the Epworth scale.
Bottom Line
While ipratropium bromide won’t replace CPAP for most moderate‑to‑severe cases, it offers a low‑cost, low‑risk option that can shave off a handful of breathing pauses each night. The emerging evidence-especially the 2023 UK RCT-suggests it’s worth a trial for anyone struggling with CPAP compliance or looking for a gentler start.
Can I use over‑the‑counter ipratropium for sleep apnea?
No. In the UK ipratropium is prescription‑only. You’ll need a clinician to assess whether it’s appropriate for your sleep‑disorder.
How long does it take to notice an improvement?
Most trials reported a noticeable drop in snoring and daytime sleepiness after about two weeks of nightly use.
Is there a risk of worsening asthma if I use it for OSA?
The risk is low. Ipratropium is actually an asthma medication, so it can help control bronchoconstriction rather than worsen it.
Can I combine ipratropium with a CPAP machine?
Yes. Some studies used a low‑level CPAP alongside ipratropium and saw additive benefits. Always discuss the combination with your sleep specialist.
What should I do if I experience dry mouth or nasal irritation?
Stay hydrated, use a humidifier in the bedroom, or switch to a milder formulation. If symptoms persist, stop the medication and seek medical advice.

Megan Dicochea
October 24, 2025 AT 12:33Anticholinergics like ipratropium block muscarinic receptors in the airway which reduces excess mucus production
That can help keep the upper airway less prone to collapse during sleep
It’s not a magic fix but it may lower the apnea‑hypopnea index a bit
Patients should still consider CPAP or positional therapy as first‑line options
Talk to a sleep specialist before adding any inhaler to your nightly routine
Jennie Smith
October 24, 2025 AT 17:33Wow the idea of repurposing an asthma inhaler for snore‑silencing is pretty rad
Imagine the night‑time symphony turning into a hush of steady breaths
The studies hint at a modest drop in events which could be a game changer for light OSA
Even if the effect is subtle, the low side‑effect profile makes it worth a trial
Just keep the device handy and monitor your sleep scores over a few weeks
Greg Galivan
October 24, 2025 AT 21:43Honestly this whole ipratropium hype is overrated and probably won’t fix severe apnea
Anurag Ranjan
October 25, 2025 AT 01:20While ipratropium isn’t a cure it can modestly reduce upper‑airway resistance in mild cases
James Doyle
October 25, 2025 AT 05:13The pharmacodynamic profile of ipratropium bromide positions it as a competitive antagonist at muscarinic M3 receptors within the bronchial epithelium. By attenuating cholinergic-mediated bronchoconstriction it reduces airway smooth muscle tone, which theoretically extends to the pharyngeal musculature. Moreover, the anticholinergic action curtails parasympathetic-driven mucosal secretions, potentially diminishing the edematous swelling that predisposes to airway occlusion. Randomized controlled trials, albeit limited in scale, have reported mean reductions in apnea–hypopnea index ranging from eight to fourteen events per hour. These findings, while modest, suggest a dose‑response relationship that merits further exploration in larger cohorts. The nebulized delivery format ensures deposition in the upper airway, contrasting with the inhaler’s distal bronchial targeting. Adherence rates appear favorable due to the non‑systemic nature of the drug and its limited side‑effect burden. However, clinicians must remain vigilant for anticholinergic adverse events such as dry mouth, constipation, and blurred vision, especially in polypharmacy populations. In the context of comorbid obstructive sleep apnea and chronic obstructive pulmonary disease, ipratropium may serve a dual therapeutic role. Nonetheless, it should not supplant continuous positive airway pressure therapy, which remains the gold standard for moderate to severe disease. Patient selection criteria should prioritize those with mild to moderate OSA, prominent nasal congestion, and a documented response to anticholinergic agents. Objective sleep study reassessment after a trial period is essential to quantify any incremental benefit. From a health economics perspective, the low cost of ipratropium could represent a cost‑effective adjunct in resource‑limited settings. Future research ought to integrate polysomnographic endpoints with biomarkers of airway inflammation to elucidate mechanistic pathways. Until such data are robust, clinicians are advised to present ipratropium as an off‑label option with transparent risk‑benefit counseling.
Edward Brown
October 25, 2025 AT 09:06One could argue that the pharma industry pushes any marginal benefit to create a new market niche and keep us dependent on perpetual medication cycles
ALBERT HENDERSHOT JR.
October 25, 2025 AT 13:00Great summary of the evidence! It’s helpful to see both the potential benefits and the cautions laid out clearly :)
Suzanne Carawan
October 25, 2025 AT 17:10Oh sure, because adding another inhaler to your nightstand is exactly what the world needs for better sleep
Kala Rani
October 25, 2025 AT 20:46Maybe if we all stopped snoring the planet would finally get some quiet nights
eko lennon
October 26, 2025 AT 00:40The night sky has always been a canvas of mystery and now we have another layer of intrigue with ipratropium stepping onto the stage of sleep medicine
Picture the drama of a restless sleeper finally finding a sigh of relief as the nebulized mist gently coats the airway like a soft veil
It’s almost cinematic how a drug born for wheezing lungs might now whisper lullabies to a faltering throat
The stakes feel high because sleep is the unsung hero of health and any tool that promises to enhance it deserves a spotlight
Yet we must temper the applause with scientific rigor lest the story become a melodrama without a solid script
Sunita Basnet
October 26, 2025 AT 03:33Indeed the therapeutic potential of ipratropium aligns with airway remodeling concepts and could synergize with positional therapy for improved outcomes
Melody Barton
October 26, 2025 AT 07:26I’m all for trying new options but don’t forget the basics like weight loss and sleeping on your side they work and cost nothing
Justin Scherer
October 26, 2025 AT 11:36Curious if any studies compared ipratropium directly against weight‑loss interventions for OSA they might show additive effects
Pamela Clark
October 26, 2025 AT 15:46Well isn’t this just the latest fad, another pill to make us feel like we’re doing something while doing nothing
Diane Holding
October 26, 2025 AT 19:56Even if it’s a trend, the data suggest a measurable reduction in apnea events for a subset of patients
Cheyanne Moxley
October 27, 2025 AT 00:06Look, if you want shortcuts you’ll find them but real change comes from lifestyle overhaul not just a spray