
Warfarin saves lives. But it’s also one of the most dangerous medications if you don’t know what to avoid. One wrong meal, a common painkiller, or even a daily supplement can send your INR skyrocketing - or crash it - with serious, sometimes deadly, consequences. If you’re on warfarin, your life isn’t just about taking a pill. It’s about understanding what your body reacts to, and why.
How Warfarin Works - And Why It’s So Sensitive
Warfarin, sold under brand names like Coumadin and Jantoven, works by blocking vitamin K. That’s not a bad thing - vitamin K helps your blood clot. Too much clotting means strokes, heart attacks, or deadly blood clots in your lungs or legs. Warfarin keeps things balanced. But here’s the catch: it doesn’t take much to throw that balance off.
Your INR (International Normalized Ratio) tells doctors how long your blood takes to clot. For most people on warfarin, the target is between 2.0 and 3.0. If it’s below 2.0, you’re at risk of clots. Above 3.0? You’re bleeding too easily. And small changes in your diet, meds, or supplements can shift your INR by 0.5 to 1.5 points in just a few days. That’s not a tiny fluctuation - that’s a medical emergency waiting to happen.
Foods That Change Your INR - Especially Vitamin K
Vitamin K is the biggest dietary player in warfarin therapy. It’s not the enemy. You need it. But you need it consistent. Eating a big bowl of spinach one day and a salad with lettuce the next? That’s a recipe for unstable INR.
Here’s what’s high in vitamin K:
- Cooked kale: 1,062 mcg per cup
- Cooked spinach: 889 mcg per cup
- Cooked broccoli: 220 mcg per cup
- Cabbage: 108 mcg per cup
- Green tea: 50-100 mcg per cup (depending on steeping time)
The NHS recommends keeping your daily vitamin K intake between 60 and 80 mcg. That doesn’t mean you can’t eat these foods. It means: pick one or two sources and eat them the same amount, every day. If you normally eat a cup of broccoli with dinner, keep doing it. Don’t swap it for kale on Tuesday and lettuce on Wednesday. Consistency is your best defense.
And yes - green tea counts. One Reddit user with atrial fibrillation reported their INR dropped from 2.8 to 1.9 in three days after drinking green tea daily. Their doctor had to increase their warfarin dose by 20%. That’s not a coincidence. That’s science.
Supplements That Can Kill You (Without You Realizing)
“Natural” doesn’t mean safe. Many supplements interact with warfarin - and they don’t come with warning labels.
Here are the most dangerous ones:
- St. John’s Wort: This popular herb for depression can reduce warfarin levels by up to 50%. Your INR crashes. Clots form. You don’t feel it until it’s too late.
- Ginkgo biloba: Increases bleeding risk. A 2021 case study in the Journal of Thrombosis and Haemostasis linked ginkgo to intracranial bleeding in a warfarin user.
- Ginseng: Can either increase or decrease INR - unpredictable and dangerous.
- Garlic supplements: Not the food. The pills. They thin blood. Combine with warfarin? Higher bleeding risk.
- Coenzyme Q10: Some studies show it weakens warfarin’s effect. Others say nothing. Either way, don’t risk it.
- Vitamin E (over 400 IU/day): Can increase bleeding time. Your doctor may not even know you’re taking it.
And don’t forget multivitamins. Many contain vitamin K. If you switch brands, your INR might shift. Always check the label. And tell your pharmacist - every time you refill.
Prescription Drugs That Turn Warfarin Into a Time Bomb
Warfarin interacts with over 300 medications. That’s 10 times more than newer anticoagulants like Eliquis or Xarelto. Here are the big ones:
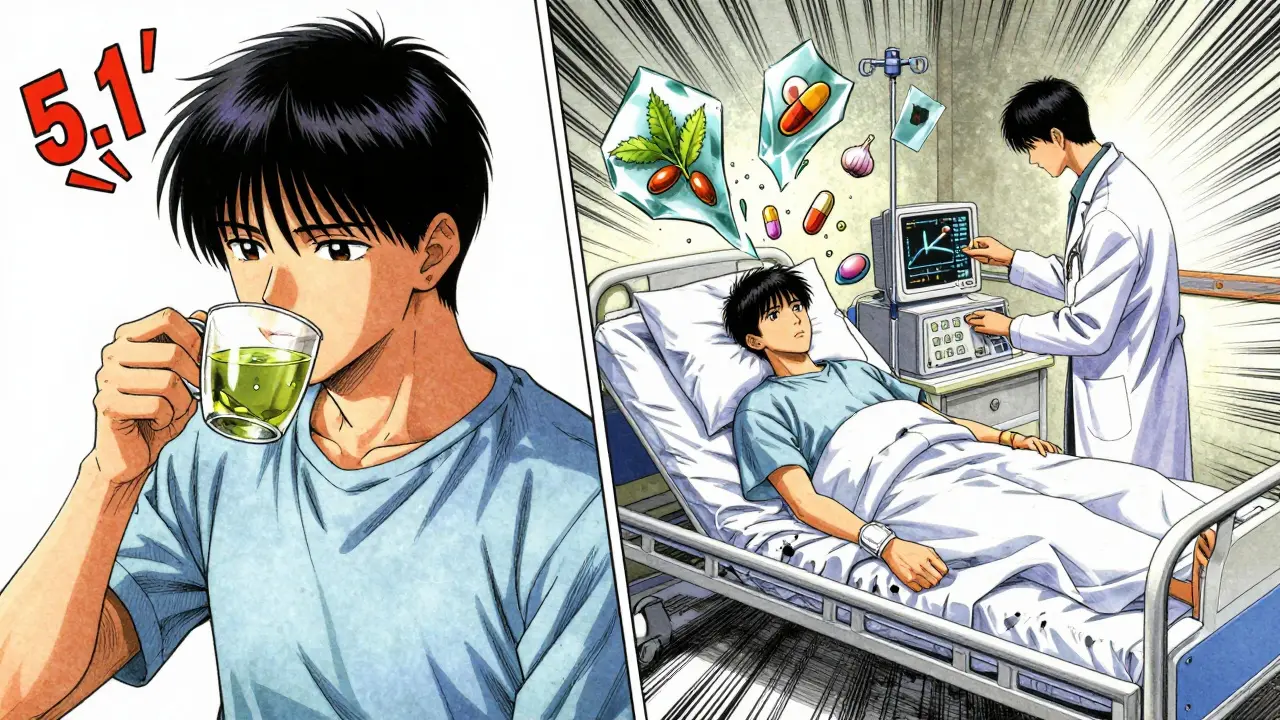
- Antibiotics: Especially Bactrim (trimethoprim-sulfamethoxazole) and ciprofloxacin. These can spike your INR by 2-3 points within days. One patient on a heart support forum had three ER visits after taking Bactrim for a UTI - their INR jumped from 2.4 to 5.1.
- Antifungals: Fluconazole (Diflucan) can increase warfarin levels by 50-100%. Your doctor should reduce your warfarin dose by 25-50% when you start this drug.
- Amiodarone: Used for irregular heartbeats. It’s one of the most dangerous combos. Studies show it increases bleeding risk by 400%.
- NSAIDs: Ibuprofen, naproxen, diclofenac - even over-the-counter ones. They irritate your stomach lining. Warfarin makes bleeding easier. Together? High risk of gastrointestinal bleeding.
- SSRIs: Like fluoxetine (Prozac) and sertraline (Zoloft). These can increase bleeding risk by interfering with platelets.
- Heartburn drugs: Omeprazole and esomeprazole can slow warfarin breakdown, raising INR.
And here’s the kicker: you might not know you’re taking one. Many prescriptions come in combination pills - like those for high blood pressure or diabetes. Always ask your pharmacist: “Does this interact with warfarin?” Don’t assume they’ll tell you.
Alcohol, Cigarettes, and Other Hidden Risks
Alcohol is tricky. One or two drinks a day? Probably fine. Three or more? Your INR spikes. The JAMA Internal Medicine 2020 study found that heavy drinking increases bleeding risk 3.2 times. And it’s not just the alcohol - it’s the pattern. Binge drinking one night and then none for a week? That’s worse than steady drinking.
Smoking? It increases how fast your body breaks down warfarin. If you quit cold turkey, your INR can rise unexpectedly. Tell your doctor if you stop smoking - they’ll likely need to adjust your dose.
What to Do - A Simple Daily Routine
Managing warfarin isn’t about fear. It’s about habits.
- Eat the same amount of vitamin K every day. Pick one green - broccoli, kale, or spinach - and stick with it. Don’t rotate.
- Never start a supplement without checking with your doctor or pharmacist. Even “harmless” ones like fish oil or ginger.
- Keep a list of every medication you take - including OTC and herbal. Bring it to every appointment.
- Get your INR checked regularly. Even if you feel fine. Stability takes weeks. One missed test can be dangerous.
- Know the signs of bleeding: Unusual bruising, nosebleeds that won’t stop, pink or red urine, black or bloody stools, severe headaches, vomiting blood.
- Use the same pharmacy. They can flag dangerous interactions before you even get the pill.

Why Warfarin Is Still Used - And When to Consider Alternatives
Why do doctors still prescribe warfarin when newer drugs like Eliquis and Xarelto exist? Because warfarin has one thing they don’t: a known antidote. Vitamin K reverses it. Prothrombin complex concentrates can stop severe bleeding fast. DOACs don’t have that. For people with mechanical heart valves - especially in the mitral position - warfarin is still the only option.
But if you’re on warfarin for atrial fibrillation and have no heart valves, ask your doctor: Is this the best choice for me? DOACs cost more - about $6,500 a year - but they don’t need monthly blood tests. Warfarin costs $80 a year, but you’ll spend hours every month at clinics. And you’ll live with constant worry about what you eat, drink, or take.
Some people say warfarin is outdated. But for millions, it’s life-saving - if managed right.
What’s New - And What’s Coming
In 2023, the FDA approved a genetic test called Warfarin GenAssist. It looks at two genes - CYP2C9 and VKORC1 - to predict how you’ll respond to warfarin. In trials, it cut the time to reach stable INR by over two weeks. That’s huge. If you’re starting warfarin now, ask if genetic testing is available.
AI tools are also emerging. A 2023 study showed machine learning models predicted warfarin dose changes with 82% accuracy - better than doctors using standard charts. These tools aren’t mainstream yet, but they’re coming.
For now, the best tool you have is knowledge. And consistency.
Can I eat leafy greens while on warfarin?
Yes - but only if you eat the same amount every day. One cup of cooked spinach daily is fine. Switching from spinach to kale to lettuce will cause your INR to swing dangerously. Consistency matters more than avoiding these foods entirely.
Is it safe to take aspirin with warfarin?
Only if your doctor specifically prescribes it. Aspirin thins blood and irritates the stomach. Combined with warfarin, it greatly increases the risk of internal bleeding. Never take it on your own - not even a low-dose baby aspirin.
How long does it take for warfarin to work?
Warfarin starts working within 24-48 hours, but it takes 3-5 days to reach full effect. That’s why doctors often start patients on a higher dose and adjust based on INR results. Don’t expect immediate results - and don’t panic if your INR is still low after a few days.
Can I drink alcohol while on warfarin?
One or two drinks per day is usually okay. But never binge drink. Three or more drinks in a short time can spike your INR and increase bleeding risk by over 3 times. Keep it consistent - and never drink heavily before an INR test.
What should I do if I miss a dose of warfarin?
If you miss a dose and remember the same day, take it right away. If you don’t remember until the next day, skip the missed dose and take your regular dose. Never double up. Keep a log of missed doses and tell your doctor at your next appointment.
Do I need to stop warfarin before surgery?
Sometimes - but never on your own. Your doctor will decide based on the type of surgery and your risk of clots. For minor procedures, you may keep taking it. For major surgery, you might switch to heparin injections temporarily. Always consult your anticoagulation clinic before any procedure.
Next Steps - What to Do Right Now
If you’re on warfarin, here’s what to do this week:
- Write down every food, supplement, and medication you take - even ginger tea or turmeric capsules.
- Call your pharmacy and ask: “Which of these interact with warfarin?” Give them your list.
- Set a reminder to eat your usual portion of vitamin K-rich food every day - same time, same amount.
- Book your next INR test - don’t wait until you feel off.
- Ask your doctor: “Is there a reason I’m on warfarin instead of a DOAC?”
Warfarin isn’t going away. For many, it’s the best option. But it demands respect. You’re not just taking a pill. You’re managing a delicate balance - every day, with every bite, every pill, every drink. Get it right, and you’ll live well. Get it wrong, and the consequences are real. Knowledge isn’t just helpful - it’s your lifeline.

Doreen Pachificus
January 4, 2026 AT 22:30Been on warfarin for 7 years. The biggest thing? Consistency. I eat the same spinach salad every Tuesday and Friday. No more guessing. My INR stays stable and I don’t stress about every leafy green I see.
Also, green tea? I switched to chamomile. No more surprises.
Akshaya Gandra _ Student - EastCaryMS
January 5, 2026 AT 01:30OMG i just realized i been takin ginkgo biloba for my memory and didnt know it was dangerous with warfarin 😳
gonna call my dr tomorrow fr
en Max
January 5, 2026 AT 12:19It is imperative to underscore that warfarin’s narrow therapeutic index necessitates vigilant pharmacokinetic monitoring, particularly in the context of concomitant medication use.
Antibiotics such as trimethoprim-sulfamethoxazole inhibit CYP2C9-mediated metabolism, thereby potentiating anticoagulant effect-this is not anecdotal; it is pharmacologically robust.
Furthermore, the variability in vitamin K content across dietary sources-particularly in leafy greens-introduces an unacceptably high degree of INR instability unless standardized intake is enforced.
Pharmacists are the frontline defense in this context. Always consult them prior to initiating any OTC agent, including herbal supplements, which are neither regulated nor inert.
Genetic testing for CYP2C9/VKORC1 polymorphisms is now standard-of-care in many institutions; if not offered, request it.
DOACs are not universally superior. In patients with mechanical mitral valves, warfarin remains the gold standard-this is not a matter of preference, but of evidence-based guidelines.
Consistency, education, and interdisciplinary collaboration are not buzzwords-they are survival protocols.
Peyton Feuer
January 6, 2026 AT 00:34lol i took ibuprofen for a headache last week and my arm turned purple. didn’t connect the dots till now.
thanks for the warning. gonna switch to tylenol from now on.
Shanna Sung
January 6, 2026 AT 20:11They don’t want you to know this but the FDA is hiding the truth about warfarin. It’s not the food or the supplements-it’s the pharmaceutical companies pushing this to keep you coming back for blood tests and expensive meds.
They don’t want you to use vitamin C or apple cider vinegar to naturally thin your blood. They profit off your fear.
My cousin’s neighbor’s dog got off warfarin and now it runs faster. Coincidence? I think not.
Allen Ye
January 7, 2026 AT 08:12Warfarin is more than a drug-it’s a philosophical confrontation with mortality.
We live in a culture that demands instant gratification: quick fixes, magic pills, no restrictions. But warfarin forces you into a rhythm-a daily ritual of balance, patience, and humility.
It asks: Can you eat the same broccoli every night? Can you resist the allure of ‘natural’ remedies that promise freedom but deliver chaos? Can you accept that your body is not a machine to be optimized, but a delicate ecosystem to be tended?
Modern medicine loves to replace warfarin with sleeker alternatives, but those drugs are silent. They don’t teach. They don’t transform. They just… work.
Warfarin, in its brutal honesty, turns compliance into wisdom. And wisdom, unlike a pill, cannot be patented.
So yes-eat your spinach. Write it down. Call your pharmacist. And thank your doctor for not giving you the easy way out.
John Ross
January 8, 2026 AT 15:14Stop acting like this is some groundbreaking revelation. This is basic clinical pharmacology taught in med school year one.
Anyone on warfarin who doesn’t know about vitamin K, St. John’s Wort, or NSAID risks is either negligent or dangerously uninformed.
And don’t get me started on people who think ‘natural’ means safe. Ginger? Fish oil? Turmeric? All anticoagulants. You’re not a holistic healer-you’re a walking bleeding risk.
If you can’t manage this, get on a DOAC. Stop wasting everyone’s time.
Clint Moser
January 9, 2026 AT 11:12Did you know the CDC is quietly pushing DOACs because they’re more profitable? Warfarin is cheaper but harder to monitor-so they want you off it.
And what about the vitamin K in multivitamins? They don’t list it on the label because they don’t want you to know.
I checked my bottle-150mcg per serving. That’s double the NHS limit. My INR spiked after switching brands. I’m not crazy. The system is rigged.
Ashley Viñas
January 10, 2026 AT 19:58Ugh. I’m so tired of people treating warfarin like it’s a diet plan. You don’t ‘eat consistent greens’-you follow your doctor’s instructions.
And if you’re taking ginkgo or garlic supplements? You’re not ‘natural’-you’re irresponsible. People die from this.
Get your INR checked. Stop Googling. Stop listening to Reddit. Your life isn’t a TikTok trend.
I’m a nurse. I’ve seen the ERs. Don’t be the person who says ‘I didn’t know’-because you did. You just didn’t care enough.