QT Prolongation Risk Calculator
Citalopram/Escitalopram QT Risk Calculator
Key Safety Thresholds: • Absolute QTc > 500ms or change > 60ms from baseline may indicate high risk • FDA/MHRA limits: Citalopram max 40mg (adults), 20mg (65+); Escitalopram max 20mg (adults), 10mg (65+)
When you’re prescribed an antidepressant, the focus is usually on how well it lifts your mood, reduces anxiety, or helps you sleep. But there’s a quiet, hidden risk that doesn’t show up in symptom checklists - a change in your heart’s electrical rhythm. For citalopram and escitalopram, two of the most commonly prescribed SSRIs, this risk is real, measurable, and strictly regulated. It’s not about feeling dizzy or having a racing pulse. It’s about something invisible on an ECG: a prolonged QT interval.
What Exactly Is QT Prolongation?
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes for your heart’s lower chambers (ventricles) to recharge between beats. If this interval gets too long, your heart can develop dangerous rhythms like Torsade de Pointes - a type of irregular heartbeat that can lead to fainting, seizures, or even sudden death. It’s rare, but it’s not theoretical. The FDA, MHRA, and other global health agencies flagged this risk after reviewing clinical data in 2011.
Both citalopram and escitalopram block a specific potassium channel in heart cells called hERG. This slows down the repolarization phase, making the QT interval stretch. The longer it stretches, the higher the chance of a dangerous rhythm. The key is understanding how much each drug stretches it - and at what dose.
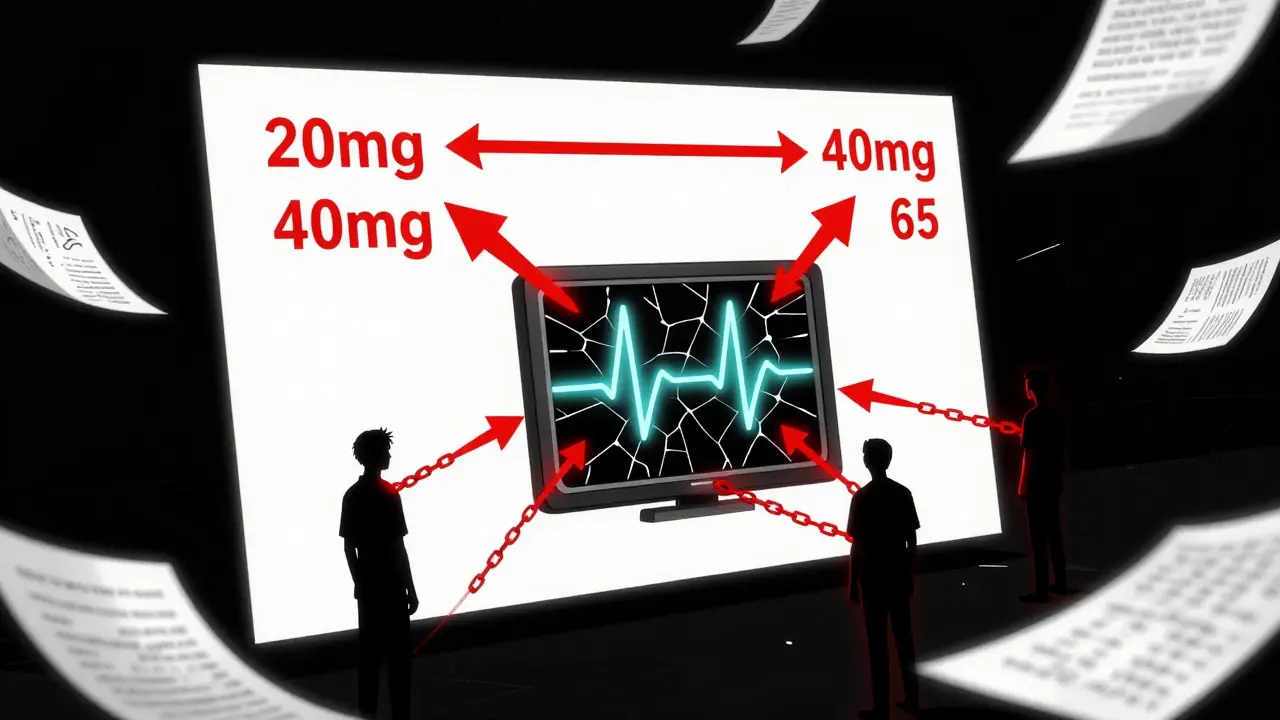
Dose Matters: The Numbers Behind the Risk
It’s not just about taking any dose. The risk rises sharply with higher amounts. Here’s what the data shows:
- Citalopram 20mg/day: QTc increases by about 8.5 milliseconds (ms)
- Citalopram 40mg/day: QTc increases by 12.6 ms
- Citalopram 60mg/day: QTc increases by 18.5 ms
For escitalopram, the effect is smaller but still present:
- Escitalopram 10mg/day: QTc increases by 4.5 ms
- Escitalopram 20mg/day: QTc increases by 6.6 ms
- Escitalopram 30mg/day: QTc increases by 10.7 ms
These aren’t guesses. They come from controlled studies and were used by regulators to set limits. The threshold for clinical concern? An absolute QTc over 500ms, or a change from baseline of more than 60ms. Most people on standard doses won’t hit that. But some will - especially if they’re older, have other heart conditions, or are taking other drugs that also affect the QT interval.
Why the Difference Between Citalopram and Escitalopram?
Citalopram is a mix of two mirror-image molecules - the R and S forms. Only the S-form is active as an antidepressant. Escitalopram is just that S-form, purified. That’s why escitalopram works at half the dose and has fewer side effects overall.
But here’s the twist: the R-form in citalopram isn’t just inactive. It actually interferes with the S-form’s action and contributes to QT prolongation. So even though escitalopram is chemically cleaner, both drugs still carry cardiac risk - just at different levels. At 40mg, citalopram pushes QTc further than escitalopram does at 20mg. That’s why many clinicians now prefer escitalopram, especially in patients with heart conditions or those over 65.
Regulatory Limits: What You Can and Can’t Take
After the 2011 safety reviews, regulators didn’t pull these drugs off the market. They set hard limits. These aren’t suggestions - they’re rules.
In the UK, the MHRA updated guidelines in December 2011:
- Citalopram: Max 20mg daily for patients over 65; max 40mg daily for adults under 65
- Escitalopram: Max 10mg daily for patients over 65; max 20mg daily for adults under 65
The U.S. FDA took a similar but narrower approach - it only restricted citalopram, not escitalopram, because the data showed escitalopram’s effect was consistently lower. Health Canada did the same. But Europe, including the UK, treated both drugs with equal caution. Why? Because even small QT prolongation can be dangerous in vulnerable people.
Age isn’t the only factor. If you have liver problems, your body clears these drugs slower. That means even a normal dose can build up to dangerous levels. Same if you’re taking other medications - antibiotics like moxifloxacin, antifungals like fluconazole, or even some anti-nausea drugs. These can stack up with citalopram or escitalopram and push your QT interval over the edge.
Who’s at Highest Risk?
Not everyone needs to avoid these drugs. But if you have any of these, your doctor should think twice:
- Age 65 or older
- History of heart disease, heart failure, or previous arrhythmia
- Low potassium or magnesium levels (common in people on diuretics or with eating disorders)
- Family history of long QT syndrome or sudden cardiac death
- Already taking other QT-prolonging drugs
- Slow heart rate (bradycardia)
People with congenital long QT syndrome should avoid both drugs entirely. If you’ve ever had unexplained fainting, especially during exercise or stress, that’s a red flag. Don’t assume it was just dehydration. Get an ECG before starting treatment.
How Do Other Antidepressants Compare?
Not all SSRIs are created equal when it comes to heart risks.
- Fluoxetine, sertraline, paroxetine: Minimal QT effect. Often safer choices for patients with cardiac concerns.
- Venlafaxine (SNRI): Low risk at normal doses, but overdose can be dangerous - especially in older adults.
- Tricyclic antidepressants (TCAs): Like amitriptyline and maprotiline - these carry higher QT prolongation risk than even citalopram. They’re rarely first-line anymore for this reason.
If your doctor is considering switching you off citalopram or escitalopram, it’s not because they’re unsafe. It’s because there are better options for your specific situation.
What Should You Do?
If you’re taking citalopram or escitalopram:
- Never increase your dose without talking to your doctor
- Don’t stop suddenly - withdrawal can be dangerous too
- Ask for a baseline ECG if you’re over 65 or have heart risk factors
- Get your electrolytes checked if you’re on diuretics or have vomiting/diarrhea
- Report dizziness, palpitations, or fainting immediately
The goal isn’t to scare you off these medications. It’s to use them wisely. For most people, the benefits far outweigh the risks. But for a small group - especially those with multiple risk factors - even a 10ms increase can tip the balance.
Is This Risk Manageable?
Yes. Studies show that when doctors follow the updated guidelines - sticking to dose limits, screening for risk factors, and avoiding drug combinations - serious events are extremely rare. The PMC9468567 study found that while QT prolongation is real, the actual risk of cardiac arrest or Torsade de Pointes in patients on these drugs remains low in clinical practice.
That’s why these medications are still among the most prescribed worldwide. The warnings didn’t kill their use - they made prescribing smarter.
What’s changed since 2011? We don’t just look at depression symptoms anymore. We look at the whole person - their age, their heart, their other meds, their labs. That’s better medicine. And it’s why you’re more likely to get the right drug, at the right dose, with the right monitoring - not just the first one on the list.
Can I take citalopram or escitalopram if I have a history of heart problems?
If you have a history of heart disease, arrhythmias, or prior QT prolongation, these medications are not automatically off-limits - but they require careful review. Your doctor should check your current ECG, review your medications, and possibly check your potassium and magnesium levels. Escitalopram is often preferred over citalopram due to its lower risk profile. In some cases, alternatives like sertraline or fluoxetine may be safer. Never start or change doses without cardiac clearance.
Why is the maximum dose for citalopram lower in older adults?
As we age, liver and kidney function decline, which slows how quickly the body clears citalopram. This means the drug builds up in the bloodstream at standard doses, increasing the risk of QT prolongation. The MHRA and FDA recommend citalopram be capped at 20mg daily for people over 65 to prevent toxic levels. The same applies to escitalopram, which is limited to 10mg daily in this group.
Is escitalopram always safer than citalopram?
In terms of QT prolongation, yes - escitalopram consistently shows a smaller effect on the QT interval at equivalent antidepressant doses. At 20mg, escitalopram causes about half the QT prolongation of 40mg citalopram. For patients with cardiac risk factors, this makes escitalopram the preferred choice. However, both drugs carry some risk, and neither should be used above recommended doses. Cost and availability may influence choice, but safety should guide the decision.
Do I need an ECG before starting these medications?
Guidelines don’t require an ECG for everyone, but it’s strongly recommended if you’re over 65, have heart disease, are on other QT-prolonging drugs, or have symptoms like dizziness or fainting. A baseline ECG helps your doctor spot pre-existing prolongation and monitor changes over time. If your QTc is already over 450ms (men) or 470ms (women), these drugs may not be safe for you.
What if I’m taking other medications along with citalopram or escitalopram?
Many common drugs can increase QT prolongation risk when combined with these SSRIs. These include certain antibiotics (moxifloxacin), antifungals (fluconazole), anti-nausea drugs (ondansetron), and some antipsychotics. Always tell your doctor and pharmacist about every medication - including over-the-counter and herbal products. Some combinations can push your QT interval into danger zone even at low doses. A simple drug interaction checker can help avoid this.
