
Most people think too much iron is a good thing - after all, iron helps carry oxygen in your blood. But when your body can’t get rid of the extra iron, it starts building up in your liver, heart, and pancreas. That’s hemochromatosis. It’s not rare. In the UK and Ireland, about 1 in 83 people carry the gene that causes it. And yet, most don’t know they have it until their liver is already damaged.
Why Your Body Can’t Handle Extra Iron
Normal iron levels? Around 0.8 to 1.2 grams total in your whole body. In someone with untreated hemochromatosis? It can hit 5 grams or more. That’s five times too much. And it doesn’t come from eating too much steak. It comes from a broken gene - usually the HFE gene, specifically the C282Y mutation. This gene tells your gut how much iron to absorb. When it’s faulty, your body keeps sucking in iron like a vacuum, even when it’s already full.
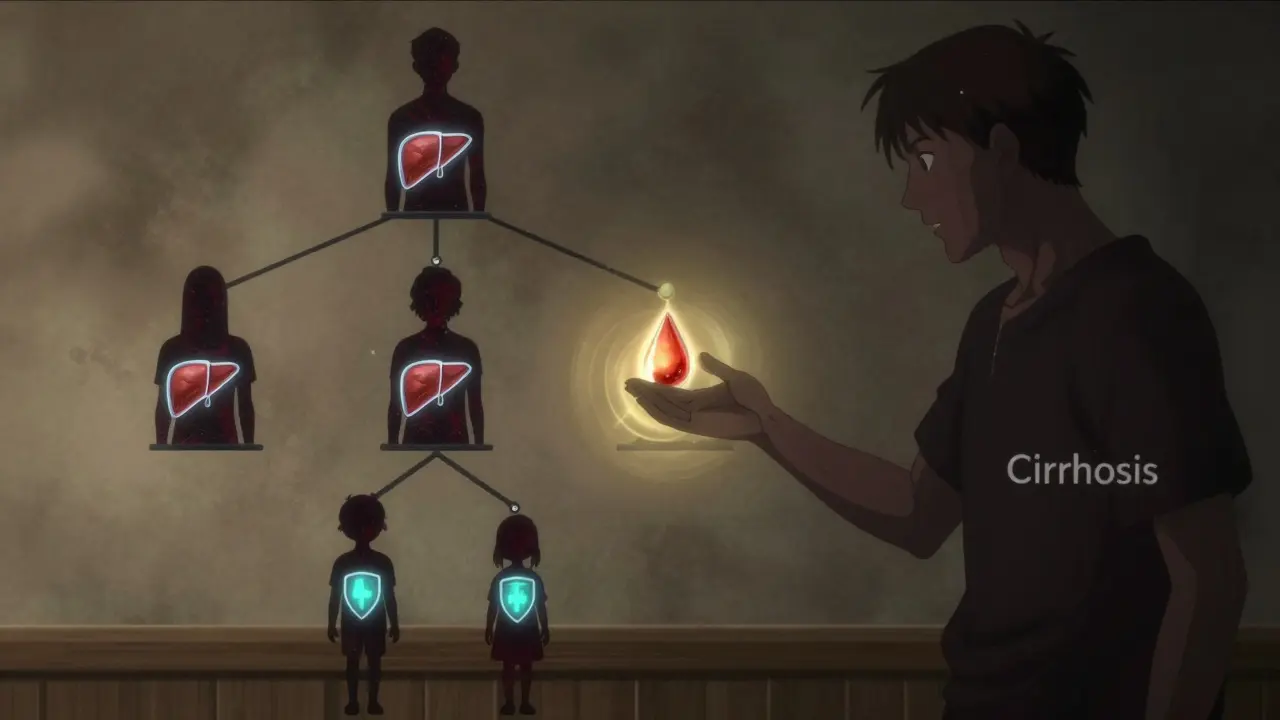
The liver is the first to suffer. Iron builds up in liver cells, causing inflammation. Over years, that turns into scarring - fibrosis. Then cirrhosis. Once cirrhosis sets in, your liver can’t heal itself. And the risk of liver cancer shoots up. By the time someone’s ferritin level hits 1,000 ng/mL, they have a 50-75% chance of already having cirrhosis. That’s why waiting for symptoms is dangerous.
What Symptoms Actually Look Like (Before It’s Too Late)
Early signs are sneaky. Fatigue? Common. Joint pain? Everyone gets that. But if you’re a man in your 40s with unexplained tiredness, aching knuckles, and low sex drive, it’s not just stress. Studies show 74% of people with hemochromatosis report extreme fatigue. Sixty-five percent have joint pain - especially in the fingers and knees. And over half have lost their libido or can’t get an erection. These aren’t normal aging signs. They’re red flags.
Later, your skin turns bronze or gray. Not from sun exposure. From iron staining your skin cells. You might get abdominal pain or even diabetes, because iron destroys the insulin-producing cells in your pancreas. By then, the damage is often permanent.
How Doctors Diagnose It (And Why Most Miss It)
Too many patients see five doctors over seven years before getting the right diagnosis. Why? Because doctors don’t test for it. They see fatigue and think depression. They see joint pain and blame arthritis. They see elevated liver enzymes and assume it’s alcohol or fatty liver.
The real test is simple: two blood numbers. First, transferrin saturation - that’s how much iron is floating in your blood. If it’s above 45%, something’s wrong. Second, serum ferritin - that’s your body’s iron storage level. Above 300 ng/mL in men, or 200 ng/mL in women, and you need genetic testing. The HFE gene test is cheap now - under £200. It’s not a fancy scan. It’s a blood tube and a DNA chip.
And here’s the kicker: if you have a close relative with hemochromatosis, you should get tested. About 70% of cases are found this way. One person gets diagnosed - their siblings and kids get tested. That’s how you stop the chain.
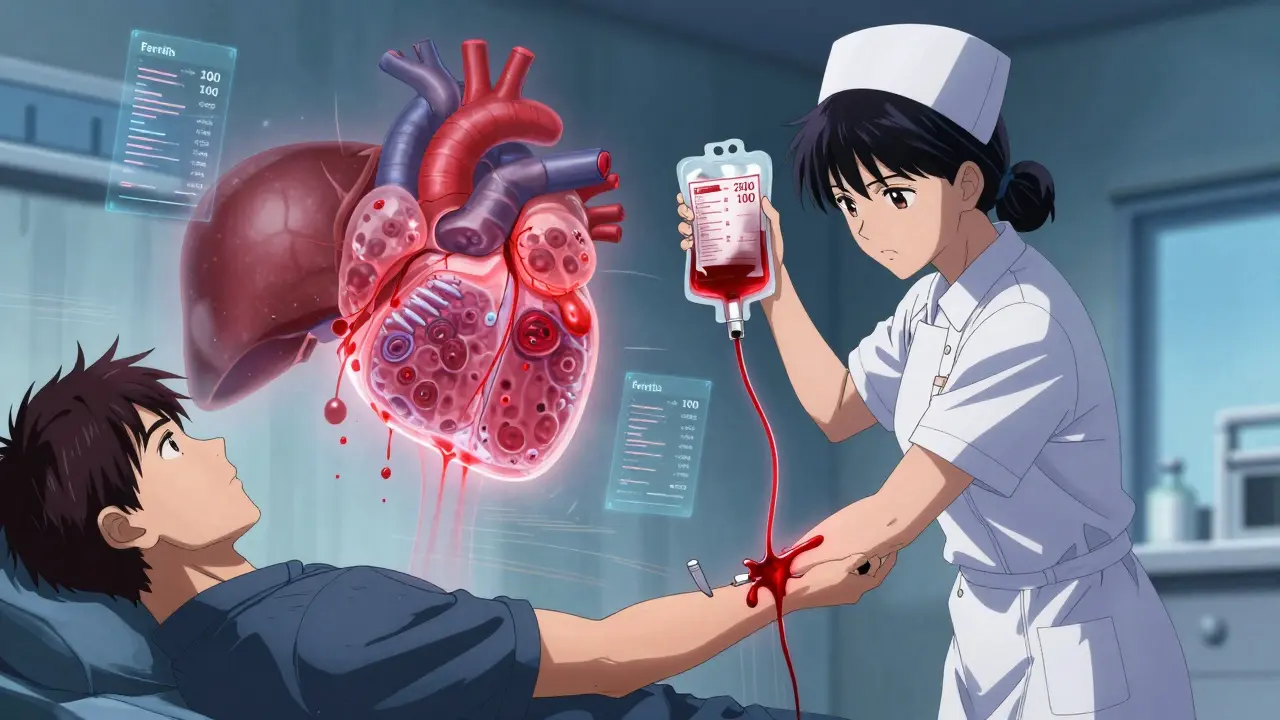
Phlebotomy: The Treatment That’s Been Working Since the 1950s
The cure? Remove the iron. Not with pills. Not with magic. With a needle. Phlebotomy - the same process as donating blood. Every week, about 450-500 mL of blood is taken. That’s 200-250 mg of iron removed. Your body doesn’t make more iron to replace it. So over time, the excess drains out.
For someone with ferritin at 2,500 ng/mL, it might take 60 sessions over 18 months to get down to safe levels. One Reddit user, u/HemoWarrior, needed 62 sessions. He said it was exhausting - but worth it. Afterward, his joint pain vanished. His energy came back. His liver enzymes normalized.
Once iron levels are under control, you switch to maintenance. Four to six phlebotomies a year. That’s it. No lifelong drugs. No expensive treatments. Just a regular blood draw. Most insurance in the UK covers it. Some NHS trusts even let you donate blood for therapeutic reasons - so you’re helping others while saving your own life.
What Happens If You Don’t Treat It
Untreated hemochromatosis doesn’t just hurt your liver. It wrecks your heart. Iron builds up in heart muscle, leading to arrhythmias or heart failure. It kills your pancreas, causing diabetes. It shuts down your pituitary gland, leading to low testosterone or early menopause. It can even cause arthritis so bad you can’t grip a cup.
And survival? If you’re diagnosed before ferritin hits 1,000 ng/mL, your 10-year survival rate is 95%. If you’re diagnosed after cirrhosis? It drops to 60%. That’s not a small difference. That’s the difference between living a normal life and needing a transplant.
Alternatives to Phlebotomy? Not Really
Some people can’t have phlebotomy - maybe they’re anemic, or have heart failure. For them, iron chelators like deferasirox exist. But they cost £25,000 a year. They come with nausea, diarrhea, and kidney risks. And they’re not as effective at clearing liver iron as regular blood removal.
There’s new research on hepcidin mimetics - drugs that trick the body into thinking it has enough iron. One drug, PTG-300, showed a 53% drop in transferrin saturation in early trials. But it’s still experimental. Not approved. Not available. Phlebotomy is still the gold standard. Simple. Safe. Free, if you’re lucky.
Living With It: What Comes After Diagnosis
Once you’re on maintenance, you’re not done. You still need to avoid iron supplements. No vitamin C with meals - it boosts iron absorption. No raw shellfish - it can carry bacteria that thrive in iron-rich blood. And no alcohol. Alcohol plus iron is a death combo for the liver.
Regular blood tests every 6 months. Ferritin checked. Liver enzymes watched. Diabetes screened. You might need to see an endocrinologist for low testosterone. A cardiologist if your heart’s affected. It’s not just one doctor. It’s a team. But it’s manageable.
Most people who stick with treatment live full lives. No transplant. No early death. Just a routine blood draw twice a year. That’s it.
Why This Isn’t Common Knowledge
It’s not a glamorous disease. No celebrity campaigns. No viral TikTok stories. It’s quiet. It creeps in. And because it’s genetic, it doesn’t spread like a virus - it hides in families. But it’s one of the most treatable genetic disorders out there. If caught early, it’s a non-issue. If missed, it’s a tragedy.
So if you’re tired all the time. If your joints ache for no reason. If you’re a man over 30 with unexplained health issues - ask for a ferritin test. Ask for transferrin saturation. Don’t wait for the skin to turn gray. Don’t wait for the liver to fail. One simple blood test could change everything.
Can hemochromatosis be cured?
Hemochromatosis can’t be cured - because it’s genetic - but it can be completely controlled. With regular phlebotomy, iron levels stay in a safe range, organs stop being damaged, and life expectancy returns to normal. Once iron is under control, most people live just as long as anyone else.
Is phlebotomy safe?
Yes, it’s very safe. It’s the same as donating blood. You might feel a little dizzy afterward, but that passes quickly. Serious side effects are rare. The bigger risk is not doing it. If you avoid phlebotomy because you’re scared of needles, you’re putting your liver, heart, and pancreas at serious risk.
Can I still eat red meat if I have hemochromatosis?
You can eat red meat, but not in large amounts. The problem isn’t the meat itself - it’s that your body absorbs too much iron from it. Stick to moderate portions. Avoid iron-fortified cereals and supplements. And never take vitamin C pills with meals - it makes your body absorb even more iron.
How often do I need phlebotomy after diagnosis?
After the initial iron removal (which can take over a year), you’ll need maintenance phlebotomy every 2 to 4 months. Most people need 4 to 6 sessions per year to keep ferritin between 50 and 100 ng/mL. Your doctor will adjust based on your blood tests.
Should my family be tested if I have hemochromatosis?
Absolutely. First-degree relatives - parents, siblings, children - have a 25% chance of having the same gene mutation. Testing them early can prevent organ damage before it starts. Many people only find out they have it because a family member was diagnosed. Don’t wait for symptoms.
Can women get hemochromatosis too?
Yes, but women are often diagnosed later. Menstruation and pregnancy naturally lower iron levels, so symptoms appear 10 to 20 years later than in men. By the time a woman is post-menopausal, she’s lost that protective effect. That’s why women over 50 with unexplained fatigue or joint pain should get tested.
Does alcohol make hemochromatosis worse?
Yes. Alcohol increases iron absorption and directly damages liver cells. When you combine alcohol with iron overload, your liver breaks down faster. Even moderate drinking can push you into cirrhosis years earlier. If you have hemochromatosis, avoid alcohol completely.
Can I donate blood if I have hemochromatosis?
In the UK, NHS Blood and Transplant allows therapeutic phlebotomy patients to donate blood - if their ferritin is below 1,000 ng/mL and they meet other donor criteria. This means you can help others while keeping your own iron levels in check. Check with your local blood donation center - many are happy to accommodate.
What to Do Next
If you’ve read this and thought, ‘That sounds like me,’ don’t wait. Ask your GP for a serum ferritin and transferrin saturation test. No referral needed. No fancy scan. Just two blood tubes. If the numbers are high, push for HFE genetic testing. If you have a family history, get tested even if you feel fine.
Hemochromatosis isn’t a death sentence. It’s a silent thief - and phlebotomy is the only thing that can catch it in time. Don’t let it steal your liver. Don’t let it steal your energy. Get tested. Get treated. Live well.
