Explore how angioedema relates to the immune system, its triggers, diagnosis, and targeted treatments for different types of swelling.
MoreAngioedema: Causes, Types, and Treatment Overview
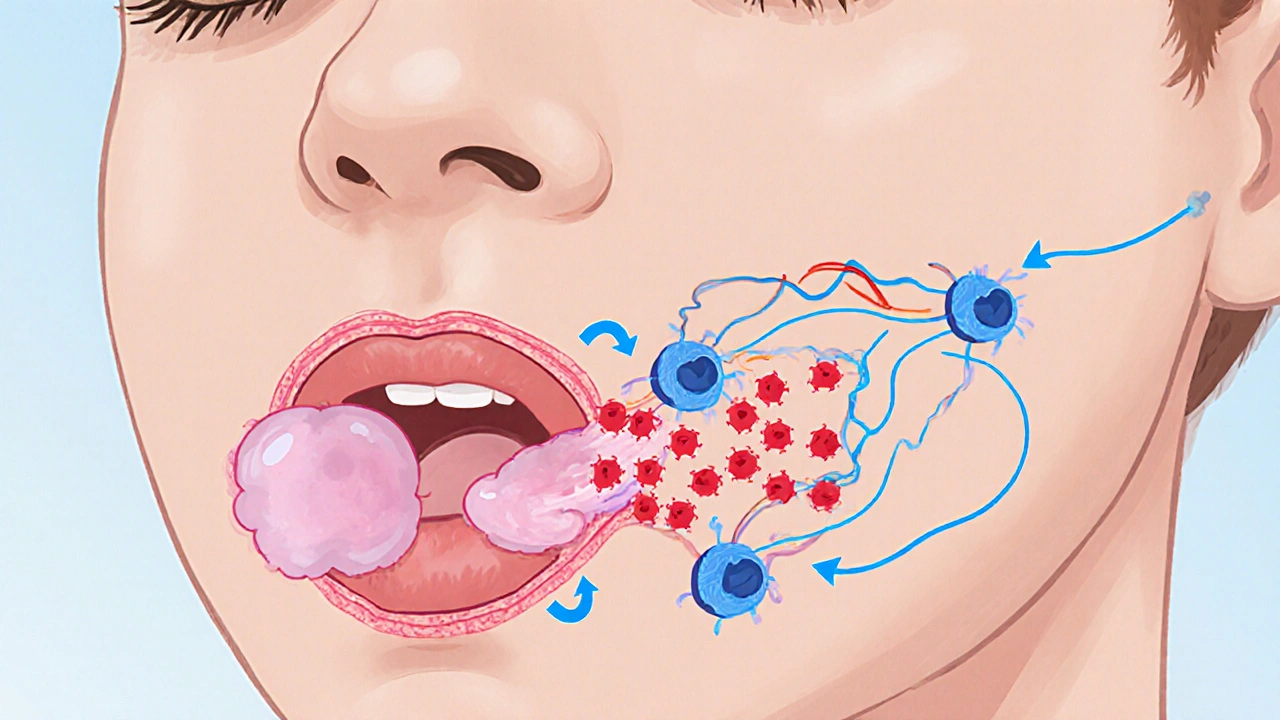
When dealing with Angioedema, a sudden swelling of the deeper layers of skin and mucous membranes that can affect the lips, eyes, throat, or gut. Also known as deep tissue swelling, it often appears without a rash and can become a medical emergency when the airway is involved. While anyone can experience an episode, certain patterns repeat often enough to deserve their own focus.
One major pattern is Hereditary Angioedema, a rare genetic condition caused by a deficiency or dysfunction of the C1 esterase inhibitor protein. This form usually starts in childhood and runs in families, with attacks triggered by stress, minor trauma, or hormonal changes. C1 Esterase Inhibitor, the protein that controls parts of the complement and contact systems, is the key molecule; when it’s missing or broken, unchecked bradykinin builds up and forces fluid into the tissues. Another frequent trigger is the class of blood‑pressure drugs called ACE Inhibitors, medications that lower blood pressure by blocking the conversion of angiotensin I to angiotensin II. By halting that conversion, they also block the breakdown of bradykinin, a peptide that widens blood vessels. Elevated bradykinin can leach fluid into the sub‑cutaneous layers, producing the classic angioedema picture. Bradykinin, a short‑lived peptide that causes blood vessels to dilate and become more permeable, is therefore a central chemical in many non‑allergic forms of angioedema.
Understanding Triggers and Mechanisms
At a high level, Angioedema encompasses three overlapping mechanisms: mast‑cell mediated allergic reactions, bradykinin‑driven drug‑induced swelling, and hereditary C1‑inhibitor deficiency. Each pathway calls for a different treatment strategy. Mast‑cell attacks respond well to antihistamines and corticosteroids, while bradykinin‑related episodes often need a quick dose of a C1‑esterase inhibitor concentrate or a bradykinin‑receptor antagonist like icatibant. Recognizing which mechanism is at work can shave minutes off the time to relief, especially in emergency rooms where airway protection is critical.
Medication side effects are a recurring theme across the PharmaShop library. For instance, articles on Lamictal dispersible versus alternatives or Symbicort versus other inhalers stress the need to read drug labels for rare adverse events. Angioedema fits that pattern: a patient taking an ACE inhibitor for hypertension might notice a subtle lip swelling that escalates after a few weeks. Knowing the link lets a clinician switch to an angiotensin‑II receptor blocker (ARB), which carries a much lower risk of angioedema while still controlling blood pressure.
Allergists often point to foods, insect stings, or latex as classic culprits. These triggers release histamine from mast cells, causing the same deep swelling but with a rash or itching that patients can usually spot. In contrast, bradykinin‑mediated swelling tends to be painless, non‑itchy, and more prolonged. This distinction matters when you’re deciding whether to reach for an epinephrine auto‑injector (ideal for allergic anaphylaxis) or a C1‑esterase inhibitor (the go‑to for hereditary or drug‑induced cases).
For those newly diagnosed with hereditary angioedema, tracking attack frequency and severity helps doctors tailor prophylactic therapy. Some patients use regular intravenous or subcutaneous C1‑esterase inhibitor replacement, while others prefer newer oral agents that block kallikrein, the enzyme that produces bradykinin. Lifestyle tweaks—avoiding extreme temperatures, managing stress, and staying hydrated—also reduce the chance of an unexpected flare.
From a pharmacy perspective, the same diligence applies to over‑the‑counter (OTC) options. Many antihistamine creams or oral tablets claim to treat “swelling,” but they only work on histamine‑driven episodes. If a patient with an ACE inhibitor tries an OTC antihistamine and sees no improvement, that’s a clue the swelling is bradykinin‑related and needs a different approach.
In emergency situations, time is the most valuable resource. The standard protocol for suspected airway‑compromising angioedema starts with securing the airway—intubation or a surgical airway if needed—followed by administering epinephrine, antihistamines, and steroids if an allergic cause is possible. If the history points to a drug like an ACE inhibitor or a hereditary pattern, clinicians add a C1‑esterase inhibitor concentrate or icatibant as soon as it’s available. This layered response reflects the semantic triple "ACE inhibitors can trigger bradykinin‑mediated angioedema" and "Hereditary angioedema requires C1‑esterase inhibitor deficiency management".
Below you’ll find a curated set of PharmaShop articles that dive deeper into related topics, from medication comparisons and safe online buying guides to condition‑specific management tips. Whether you’re a patient looking for practical steps, a caregiver seeking clear explanations, or a health professional needing quick reference points, the collection offers actionable insight into the many faces of angioedema.