
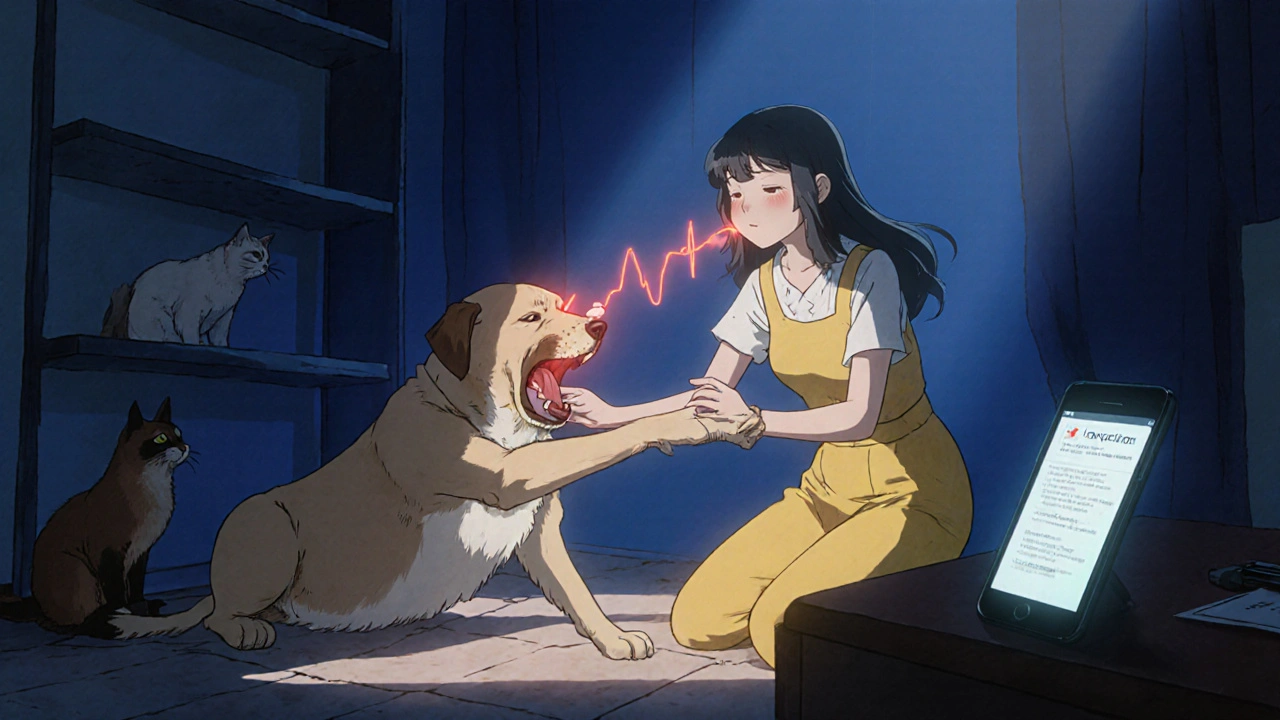
Imagine a dog nudging you moments before a seizure-like a silent alarm that could give you precious seconds to brace yourself. That scenario isn’t sci‑fi; it’s becoming a real option for many living with partial onset seizures. In this guide we’ll unpack how animals pick up on seizure cues, what training looks like, and how you can safely integrate a four‑legged (or even a feline) teammate into your seizure‑management plan.
What Exactly Are Partial Onset Seizures?
Partial onset seizure is a type of epileptic event that starts in a specific brain region before it may spread to other areas. Unlike generalized seizures that affect the whole brain, partial onset seizures often cause localized sensory changes-like a flash of light, a sudden smell, or a brief loss of muscle control on one side of the body. Because the symptoms can be subtle, many people don’t recognize them until they progress to a tonic‑clonic episode.
Key attributes of partial onset seizures include:
- Focal onset: symptoms begin in a single brain lobe.
- Varied manifestations: motor, sensory, autonomic, or psychic.
- Potential to evolve into a secondary generalized seizure.
Early detection can mean the difference between staying safe at home and ending up in the emergency room. That’s where pets come into play.
Why Pets Might Detect Seizures Before You Do
Animals, especially dogs, have an extraordinary sense of smell-up to 100,000 times more sensitive than humans. Researchers have identified volatile organic compounds (VOCs) that change in a person’s sweat or breath minutes before a seizure. These chemical shifts create a “seizure scent” that trained dogs can learn to recognize.
Beyond scent, pets pick up on subtle behavioral cues: a slight change in posture, a tremor, or an altered breathing pattern. Cats, though more independent, can also sense these changes and may respond with pawing or vocalizing.
Here’s a quick snapshot of the science:
- Olfactory biomarkers: Studies at the University of Pennsylvania found a consistent rise in acetone and isoprene levels 30 seconds before a seizure.
- EEG‑correlated behavior: Dogs have been observed to bark or whine exactly when an EEG shows early ictal activity.
- Neuro‑cardiac cues: A slight spike in heart rate can be sensed by a pet’s keen hearing of breathing changes.
Training a Seizure‑Detection Pet: From Puppy to Protector
Most seizure‑detection programs focus on dogs because their training infrastructure is well‑established. However, the basic steps apply to any animal you plan to involve.
- Select the right breed: Labrador retrievers, golden retrievers, and German shepherds dominate the field due to their eager-to‑please temperament.
- Establish a scent profile: Collect scent samples from the person during a seizure (e.g., sweat on a pillow) and create a training kit.
- Condition the alert behavior: Use positive reinforcement (treats, praise) when the dog sniffs the sample and performs a specific alert-like sitting, nudging, or pawing.
- Generalize to real‑world settings: Practice in various rooms, lighting conditions, and with background noises to ensure the dog’s alert stays reliable.
- Maintain and refresh: Monthly refresher sessions keep the scent memory sharp.
Training a cat follows similar principles but leans more on natural predatory cues-such as a sudden pounce when they detect a scent. Because cats are less likely to wear a harness, owners often use a bell‑tag to signal the cat’s presence.

How Pets Help Manage Partial Onset Seizures
Once a pet reliably alerts you, you gain a critical window to act. Here are practical steps you can take after an alert:
- Sit or lie down in a safe spot to prevent falls.
- Take any prescribed rescue medication (e.g., benzodiazepine tablets).
- Notify a caregiver or use a smart‑phone emergency app.
- Log the event’s time and trigger in a seizure diary for your neurologist.
Beyond alerts, some owners train pets to fetch a phone, turn off dangerous appliances, or even retrieve a medical alert bracelet. These supportive actions reduce injury risk and help you stay calm during a seizure.
Dog vs. Cat: Which Is Better for Seizure Detection?
| Species | Typical Training Time | Detection Accuracy (reported) | Suitability for Home Use | Maintenance Needs |
|---|---|---|---|---|
| Dog | 6‑12 months | 85‑95% | High (consistent alerts) | Daily exercise, grooming |
| Cat | 9‑18 months | 70‑80% | Medium (more independent) | Litter box, occasional play |
Dogs outshine cats in training speed and accuracy, but cats can still be valuable, especially for owners with limited space or allergies to dog dander.
Real‑World Success Stories
Buddy the Labrador saved his owner, Maya, from a near‑fatal seizure in 2022. The dog barked and pawed at Maya’s wrist five minutes before her motor aura began, allowing her to take intranasal diazepam and avoid a fall.
In another case, a Siamese cat named Luna began meowing loudly whenever her owner’s heart rate spiked-an early sign of a focal seizure. Though Luna’s alerts were less precise, they still gave her owner a chance to sit down and call emergency services.
These anecdotes illustrate that while results vary, many families experience a tangible safety boost when a pet is part of their seizure plan.
Potential Pitfalls and How to Address Them
Integrating a pet isn’t a guaranteed cure. Here are common challenges and ways to mitigate them:
- False alerts: Pets may react to other odors or noises. Fine‑tune training with “no‑alert” rounds where the scent isn’t present.
- Allergies or asthma: Choose hypoallergenic breeds (e.g., Poodles) or go with a cat if you’re sensitive to dog dander.
- Cost and time: Professional training can run $2,000‑$5,000. Some non‑profits offer subsidized programs for people with epilepsy.
- Legal considerations: In public spaces, ensure your dog’s certification is up‑to‑date to avoid access issues.
Getting Started: A Step‑by‑Step Checklist
- Consult your neurologist about adding a pet‑alert system to your care plan.
- Identify a reputable seizure‑detection training organization (e.g., Canine Companions for Independence).
- Choose a suitable pet based on living space, lifestyle, and any allergies.
- Collect scent samples during a seizure event (with medical supervision).
- Begin formal training, ensuring the pet learns a clear, consistent alert behavior.
- Set up a safety protocol-medication, emergency contacts, and a seizure diary.
- Practice the full response routine weekly until it feels automatic.
- Review and refresh training quarterly, especially after any medication changes.
Following this checklist can turn a furry friend into a reliable early‑warning system for partial onset seizures.
Frequently Asked Questions
Can any dog be trained to detect seizures?
Most breeds can learn the scent, but working breeds like Labrador retrievers and German shepherds have higher success rates due to their motivation and trainability.
How early can a pet alert before a partial onset seizure?
Research shows dogs can bark or nudge 30 seconds to 2 minutes before visible symptoms appear, giving enough time to take rescue medication.
Do cats need a harness to signal an alert?
Typically no. Many owners attach a lightweight bell‑tag or a small safety vest that the cat will wear during training, allowing the owner to recognize the alert.
Is there insurance coverage for seizure‑detection pet training?
Some health insurers reimburse part of the cost if a doctor prescribes the service; we recommend checking your policy and asking for a medical necessity letter.
What should I do if my pet gives a false alarm?
Stay calm, verify your symptoms, and if none are present, log the false alert. Use it as feedback to adjust training-often a short “no‑alert” session helps the pet fine‑tune its response.
Integrating a pet into seizure management isn’t a magic bullet, but for many living with partial onset seizures, the extra seconds of warning can be life‑changing. If you’re curious, start the conversation with your neurologist and explore reputable training programs. Your new four‑legged ally might just become your most reliable early‑warning system.

Heather ehlschide
October 23, 2025 AT 20:02Partial onset seizures can be subtle, so a reliable alert system is worth the effort.
First, confirm with your neurologist that a pet‑assisted protocol fits your medical plan.
Choose a breed or species that matches your living situation and any allergy concerns.
Collect scent samples by placing a clean gauze on your forehead during a breakthrough event, then store it in a sealed container.
Present the sample to the dog while rewarding a sit or paw with a high‑value treat; repeat until the animal consistently associates the scent with the behavior.
Gradually introduce background noises, different lighting, and other people to prevent false positives.
Practice the alert in your bedroom, kitchen, and living room, noting the exact latency between the dog’s signal and the onset of symptoms.
Record every alert in a seizure diary, including false alarms, to fine‑tune the training protocol.
Monthly refresher sessions keep the scent memory sharp and prevent drift.
If you opt for a cat, attach a lightweight bell‑tag and use a clicker to mark the moment the cat vocalizes.
Teach the cat to retrieve a phone or flash a light by rewarding the action immediately after a meow triggered by the scent.
Never rely solely on the pet; keep rescue medication within arm’s reach at all times.
Install a smart‑home routine that can be activated by the pet’s alert, such as turning off appliances or sending a text to a caregiver.
Consider insurance coverage: some policies reimburse training costs when a physician’s note is provided.
Stay patient-initial false alerts are common, but consistency will improve accuracy over weeks.
Remember that the goal is extra seconds, not a cure, and those seconds can make the difference between a safe sit and a dangerous fall.
Kajal Gupta
November 8, 2025 AT 13:02Wow, the guide really paints a vivid picture of how our furry friends can become lifesavers! I love the way you broke down the scent‑training steps into bite‑size chunks-makes the whole process feel doable.
Honestly, the idea of a cat with a bell‑tag is both adorable and surprisingly practical.
Just imagine that little “meow‑alarm” echoing through the house right before a aura hits.
For anyone worried about space, a compact apartment can still host a diligent Labrador or a sleek Siamese.
Overall, the blend of science and heartwarming anecdotes gives readers both confidence and hope.
Zachary Blackwell
November 24, 2025 AT 07:02Everyone’s quick to celebrate these “miracle pets,” but have you considered who’s really pulling the strings? Big pharma loves to keep us dependent on drugs while pet‑training outfits get hefty government grants-sounds like a coordinated distraction.
They’ll have us believing a dog’s nose is the next front‑line defense, but the real agenda is data harvesting from every sniffed sample.
Don’t be fooled by cute stories; ask yourself why the industry pushes for expensive certification programs instead of affordable open‑source scent kits.
Stay skeptical, stay informed, and don’t hand over your health to anyone’s pet agenda.
Shubhi Sahni
December 10, 2025 AT 01:02Indeed, the steps outlined are clear, comprehensive, and-most importantly-accessible; however, prospective owners should also consider logistical constraints, such as time commitments, financial investment, and the animal’s own well‑being, before embarking on training.
It is essential, therefore, to schedule regular check‑ins with a veterinary behaviorist, to monitor the pet’s stress levels, and to adjust reinforcement schedules accordingly.
Moreover, integrating a seizure‑alert routine into daily life can reinforce habit formation, both for the handler and the animal, thereby enhancing reliability over the long term.
Danielle St. Marie
December 25, 2025 AT 19:02Patriotic readers, 🇺🇸 remember that American innovation has pioneered service‑dog programs long before anyone tried to "hide" the truth behind conspiracies! 🙄 The dedication of our vets and trainers is a testament to hard work, not some shadowy “agenda.” 💪🏽 If you truly care about safety, support local nonprofits that train these heroes-don’t waste time with baseless theories.
keerthi yeligay
January 10, 2026 AT 13:02Yes, these programs are really effective, defiantly worth the cost.
Peter Richmond
January 26, 2026 AT 07:02From a cultural perspective, incorporating a trained animal into a seizure management plan respects both medical protocol and the historic bond between humans and companion animals. It also aligns with holistic approaches endorsed by many health organizations.