
Antihistamine Drowsiness Calculator
Estimated Drowsiness Duration
Have you ever taken Benadryl for allergies, only to feel so tired you couldn’t stay awake past dinner - and then still felt foggy the next morning? You’re not alone. Millions of people reach for first-generation antihistamines like diphenhydramine, chlorpheniramine, or promethazine because they’re cheap, easy to find, and seem to work fast. But what most people don’t realize is that these medications aren’t just stopping sneezes - they’re hijacking your brain.
Why You Feel Like You’ve Been Hit by a Truck
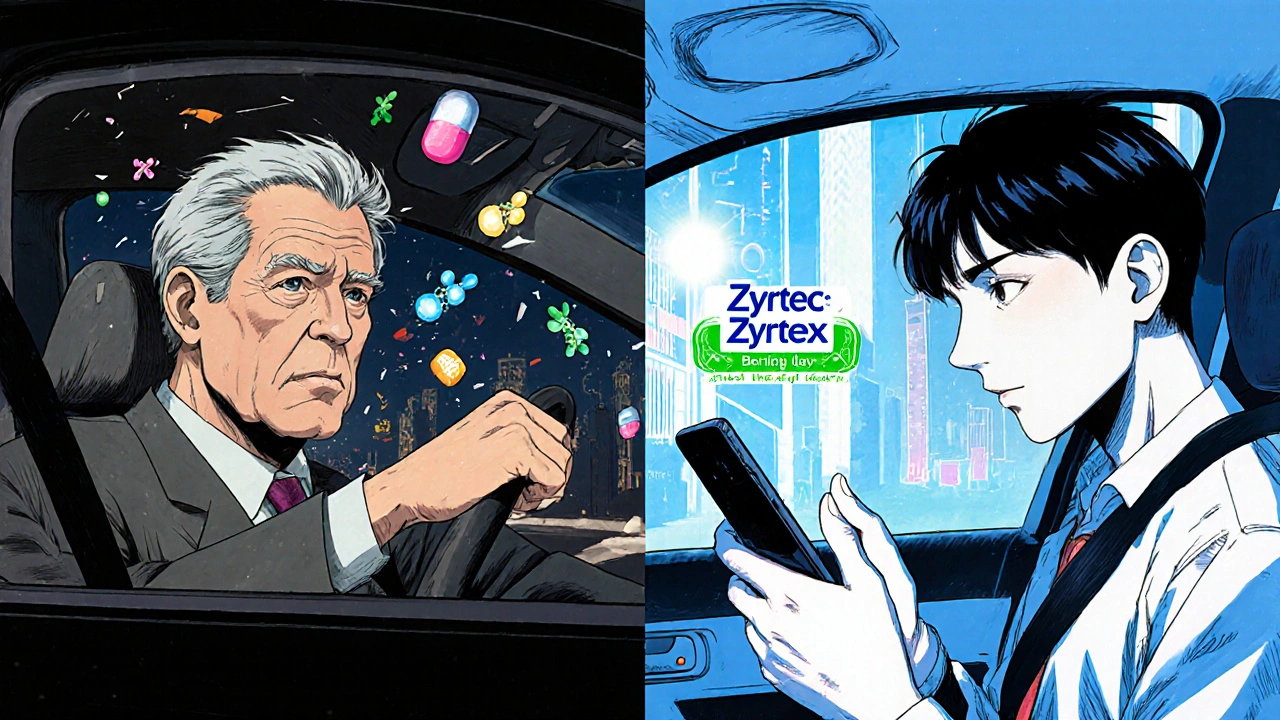
First-generation antihistamines were designed to block histamine, the chemical your body releases during an allergic reaction. But here’s the catch: they don’t stop at the nose or skin. Because they’re small and oily, they slip easily through the blood-brain barrier. Once inside your brain, they latch onto H1 receptors - the same ones that help keep you alert during the day. By shutting these down, they cause intense drowsiness.This isn’t mild sleepiness. Studies using driving simulators show that after taking a standard 25 mg dose of diphenhydramine, reaction times drop as much as if you’d had three drinks. The effects can last up to 18 hours. That’s why so many people report waking up groggy, forgetting where they put their keys, or struggling to focus at work - even if they took the pill the night before.
More Than Just Sleepiness: The Anticholinergic Side Effects
These drugs don’t just mess with histamine. They also bind to muscarinic receptors, which control things like saliva production, bladder control, and pupil size. That’s why side effects go beyond tiredness. Dry mouth? That’s one. Blurry vision? That’s two. Trouble peeing? That’s three. And for older adults, this can be dangerous.The American Geriatrics Society calls first-generation antihistamines “potentially inappropriate” for people over 65. Why? Because chronic use is linked to a 54% higher risk of cognitive decline and dementia. In one study of 1,204 older users, 42% said they felt confused for hours after taking their nightly dose. It’s not just memory - it’s attention, processing speed, and decision-making that suffer. And it doesn’t take years. Even a few months of regular use can start to show up on brain scans.
How They Compare to Second-Generation Antihistamines
Second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) were created to fix this problem. They’re bigger, less oily, and can’t cross into the brain easily. Their brain concentrations are less than 1 ng/mL - compared to 15-25 ng/mL for diphenhydramine. That means they work just as well for allergies, but you don’t feel like you’re drugged.Driving tests show second-gen antihistamines cause barely any impairment. Their sedation index? Around 0.1-0.3. For first-gen? 0.7-0.9. That’s nearly full impairment. And while first-gen drugs need to be taken every 4-6 hours, second-gen ones last 12-24 hours. One pill a day. No midday crashes.
Cost-wise, first-gen wins. A bottle of 24 diphenhydramine tablets runs about $5. The same number of cetirizine tablets? Around $15. But when you factor in lost productivity, accidents, or hospital visits from side effects, the cheaper option isn’t always the better one.
When They Still Make Sense - And When They Don’t
Let’s be fair: first-generation antihistamines aren’t all bad. They’re still the most effective option for motion sickness. If you’re on a boat or in a car that makes you nauseous, diphenhydramine or promethazine can help - and fast. They’re also the go-to for short-term insomnia. For someone who can’t fall asleep, a 25 mg dose can knock you out in 20 minutes.But here’s the line: use them once in a while, not every night. Don’t use them for daily allergies. Don’t give them to kids without a doctor’s advice. And never mix them with alcohol. Alcohol boosts brain penetration by 40-60%, turning a sleepy pill into a dangerous one.
Doctors often recommend starting with a low dose at bedtime to see how your body reacts. Many people need to cut their dose in half - especially older adults or those on other meds. If you’re taking blood pressure pills, antidepressants, or painkillers, you could be at risk for dangerous interactions. These drugs are processed by liver enzymes (CYP2D6 and CYP3A4), and if your body handles them slowly, the effects can last way longer than expected.
What Users Really Say
On Drugs.com, diphenhydramine has a 5.2 out of 10 rating from nearly 4,000 reviews. Over a third of users say they felt “extreme sleepiness.” One Reddit user wrote: “Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck - not worth it for mild allergies.”Meanwhile, older users on AgingCare.com admit they use it for sleep - but many report “morning confusion” lasting hours. Some describe needing artificial saliva because their mouth was so dry. Others say they forgot appointments, missed medication doses, or nearly crashed their car.
It’s not just anecdotal. A 2022 JAMA study found that 45% of people using these drugs underestimated how long the drowsiness would last. They thought they’d be fine by morning. They weren’t.

What’s Changing - And What to Expect
Regulators are catching up. The UK banned over-the-counter sales of promethazine to minors in 2022. The FDA is considering similar limits on diphenhydramine after pediatric ER visits jumped 27% between 2018 and 2022. New labeling rules now require stronger warnings about next-day impairment.Pharma companies are working on “third-generation” antihistamines that block allergies without touching the brain. Two are already in mid-stage trials, showing 80% less brain penetration while keeping the same allergy-fighting power.
But for now, the choice is yours. If you’re using first-gen antihistamines for allergies, you’re trading safety for savings. If you’re using them for sleep, you’re risking long-term brain health for short-term relief. And if you’re using them every day? You’re playing with fire.
What You Should Do Instead
- For allergies: Try cetirizine, loratadine, or fexofenadine. They’re non-drowsy, just as effective, and now widely available as generics.
- For sleep: Talk to your doctor about melatonin, cognitive behavioral therapy for insomnia (CBT-I), or short-term use of prescription sleep aids - not antihistamines.
- For motion sickness: Dimenhydrinate (Dramamine) is still an option, but try ginger supplements or acupressure bands first - they’re safer and work for many people.
- For chronic use: Avoid these drugs entirely. There are better, safer alternatives.
If you’re already taking a first-generation antihistamine, don’t quit cold turkey. Talk to your pharmacist or doctor. They can help you switch safely - and explain why the change matters.
Are first-generation antihistamines safe for older adults?
No. The American Geriatrics Society strongly advises against using first-generation antihistamines like diphenhydramine or promethazine in people over 65. These drugs have strong anticholinergic effects that increase the risk of confusion, falls, urinary retention, and long-term cognitive decline. Studies show chronic use raises dementia risk by 54%. Safer alternatives exist for sleep and allergies.
How long does drowsiness last after taking Benadryl?
Drowsiness from diphenhydramine typically starts within 30 minutes and peaks at 1-2 hours. But the effects don’t disappear after a few hours. Studies show cognitive impairment can last up to 18 hours, especially in older adults or those with slower metabolism. Many people feel foggy the next day without realizing why.
Can I drive after taking a first-generation antihistamine?
No. Driving after taking diphenhydramine, chlorpheniramine, or promethazine is dangerous. These drugs impair reaction time, attention, and coordination as much as alcohol. In 2021, 35% of emergency visits for drowsy driving involved first-generation antihistamines. Even if you feel fine, your brain is still impaired. Never drive after taking these meds.
Why do these drugs cause dry mouth and blurred vision?
First-generation antihistamines don’t just block histamine - they also block muscarinic receptors, which control saliva, tear, and bladder function. This is called anticholinergic activity. When these receptors are shut down, you get dry mouth, dry eyes, blurred vision, and trouble urinating. These side effects are common, predictable, and often underreported.
Are there any safe, non-drowsy alternatives to Benadryl?
Yes. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) work just as well for allergies without causing drowsiness. They don’t cross into the brain significantly, so they don’t impair cognition. Most are available as low-cost generics and can be taken once daily. For sleep, try melatonin or CBT-I instead of antihistamines.

David Cunningham
November 23, 2025 AT 06:29Been taking Benadryl for years for allergies and honestly didn’t realize how much it was wrecking my focus at work. Thought I was just a sleepy person. Turns out I was just drugged. Switched to Zyrtec last month and it’s like waking up from a coma. No more 3 p.m. naps, no more forgetting why I walked into the kitchen. Best $10 I ever spent.
Holly Schumacher
November 23, 2025 AT 10:10Let me be perfectly clear: using first-generation antihistamines as sleep aids is not just irresponsible-it’s a slow-motion neurological suicide pact. The data is irrefutable: 54% increased dementia risk? That’s not a ‘maybe,’ that’s a statistical death sentence wrapped in a $5 bottle of liquid fog. And yet, people-especially older adults-are still popping these like candy because they’re ‘convenient.’ Convenience is the new complacency, and we’re all paying for it in brain cells.
Stop romanticizing the ‘quick fix.’ Your grandmother’s generation didn’t have Zyrtec? So what? They also didn’t have MRI scans showing hippocampal atrophy from anticholinergic burden. You’re not ‘just tired’-you’re chemically sedating your prefrontal cortex. Wake up.
Melvina Zelee
November 23, 2025 AT 20:14honestly i think this post is so important but also so hard to hear. i used to take benadryl every night to sleep because i thought it was ‘natural’-like, it’s just an allergy pill right? but then i started forgetting names, missing appointments, and my husband said i’d stare at the TV like a zombie. i didn’t even realize it was the meds til i read this. switched to melatonin and cbt-i and honestly? my brain feels like it’s been cleaned. it’s not magic, but it’s better. and no, i don’t feel like a failure for needing help. we’re just not taught how to sleep well anymore.
steve o'connor
November 24, 2025 AT 02:00My dad’s a retired nurse and he still swears by diphenhydramine for sleep. I showed him the JAMA study and he just shrugged and said, ‘Well, it works.’ That’s the real problem here-people aren’t ignoring the science, they’re just tired of being told what to do. We need better education, not just more warnings.
Patrick Marsh
November 25, 2025 AT 03:14Don’t drive after taking these. Ever.
Robin Johnson
November 27, 2025 AT 00:11For anyone reading this and thinking, ‘I’m fine-I just take it once a week’-you’re not. Even occasional use adds up. Your brain doesn’t reset like a phone. The damage is cumulative. Start with one non-drowsy antihistamine this week. Don’t wait for a crash. Your future self will thank you.
Latonya Elarms-Radford
November 28, 2025 AT 22:59Oh, the tragedy of modern pharmacology-where convenience has become our collective opiate, and the quiet erosion of cognition is dismissed as ‘just aging.’ We’ve turned our brains into disposable hardware, swapping synaptic clarity for the illusion of control. Diphenhydramine isn’t a medicine-it’s a cultural surrender. We’ve normalized chemical sedation as self-care, mistaking numbness for peace. And now, we’re raising a generation that doesn’t know what clarity feels like. The real epidemic isn’t allergies-it’s our refusal to sit with discomfort, to breathe through insomnia, to feel the full weight of being human without chemical anesthesia. We don’t need better drugs. We need to remember that not every problem requires a pill. Sometimes, the most radical act is simply… to be awake.
Mark Williams
November 30, 2025 AT 20:56Key pharmacokinetic point: the CYP2D6 polymorphism significantly impacts diphenhydramine metabolism. Poor metabolizers exhibit 3–4x higher AUC and prolonged half-life, increasing anticholinergic burden. This is why older adults and those on polypharmacy are at disproportionate risk. The 54% dementia correlation isn't just epidemiological-it's mechanistic. Second-gen agents have negligible CNS penetration (IC50 > 1000 nM vs. 15–25 ng/mL for 1st-gen). Pharmacoeconomic models show that even at 3x cost, second-gen reduces long-term healthcare utilization by 18–22% due to fewer falls, ER visits, and cognitive decline. The ‘cheap’ option is a false economy.