
SSRI Side Effect Comparison Tool
Compare Your SSRI
Select your medication to see common side effects, their severity, and estimated likelihood
When you start an SSRI for depression or anxiety, you’re not just hoping for better mood-you’re also signing up for a list of possible side effects. Some are mild and fade fast. Others stick around, change your life, or even scare you. The truth? Almost 9 out of 10 people on SSRIs experience at least one side effect. And for more than half, it’s bad enough to make them question whether the drug is worth it.
What Are SSRIs, Really?
SSRIs-Selective Serotonin Reuptake Inhibitors-are the most common antidepressants in the U.S. and UK. They include drugs like sertraline (Zoloft), fluoxetine (Prozac), escitalopram (Lexapro), and paroxetine (Paxil). They work by blocking serotonin from being reabsorbed too quickly in your brain. More serotonin in the spaces between nerve cells means better mood regulation. That’s the theory. But the body doesn’t just adjust quietly. It reacts.Mild Side Effects: The First Few Weeks
Most people feel something within the first week. Nausea is the #1 complaint. About half of users get it. It’s not just a stomach ache-it’s a wave of queasiness that hits after eating, sometimes even when you haven’t eaten. Taking the pill with food cuts this down by nearly 60%, according to surveys from Psych Central. Headaches, dizziness, dry mouth, and fatigue show up too. You might feel like you’re moving through syrup. Sleep gets messed up-either you’re too tired to get out of bed, or you’re wide awake at 3 a.m. Insomnia affects 1 in 6 people. Drowsiness? That’s even more common. These aren’t signs you’re doing something wrong. They’re your body learning how to live with more serotonin. Most of these symptoms drop off after 3 to 6 weeks. A GoodRx survey found 78% of nausea cases disappear within 21 days without any change to the dose.Weight Gain: It’s Not Just in Your Head
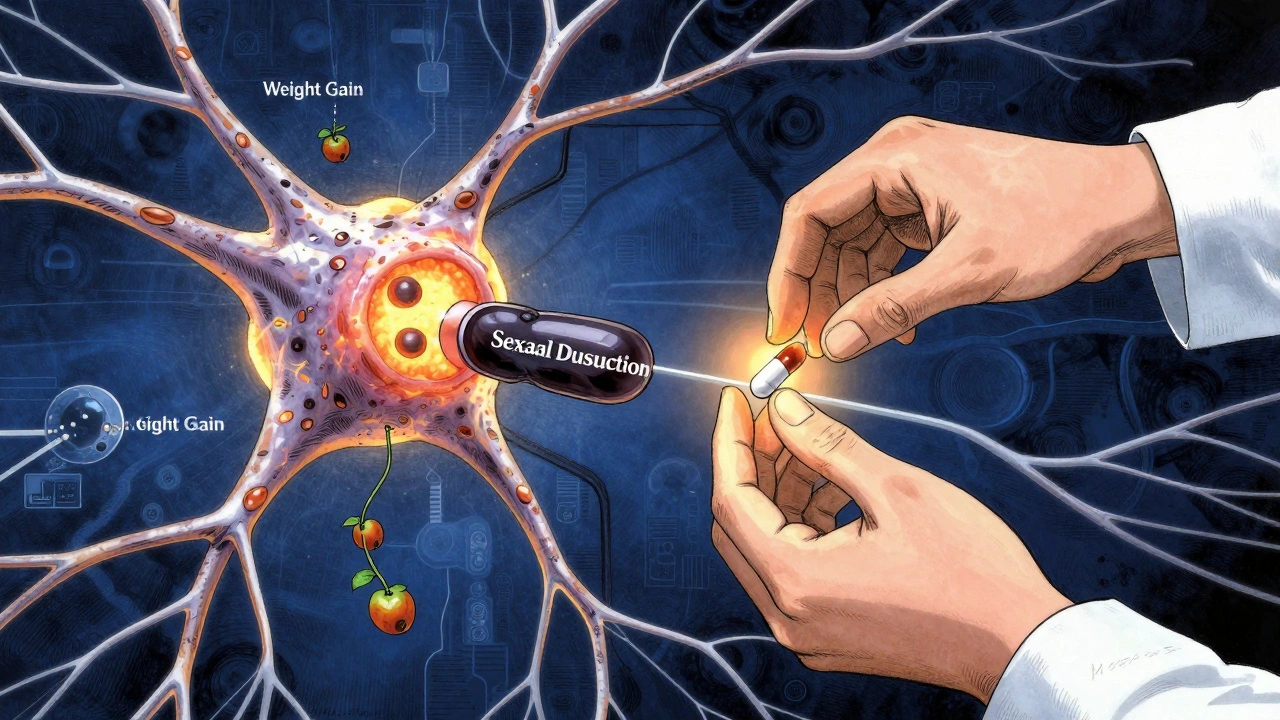
Weight gain is one of the most talked-about side effects-and one of the most misunderstood. People assume it’s just cravings or laziness. But it’s biological. SSRIs affect serotonin receptors that control appetite and metabolism. Studies show nearly half of users gain weight over time. Paroxetine and fluoxetine are the biggest culprits. In one 2023 meta-analysis, patients on these drugs gained an average of 2.5 kg in six months. But it’s not inevitable. People who added regular walking or strength training gained 3.2 kg less than those who didn’t. Eating more protein and fewer processed carbs helps too. It’s not about willpower-it’s about countering a drug-induced metabolic shift.Sexual Dysfunction: The Silent Problem
This is where things get serious. Up to 70% of people on long-term SSRIs report sexual side effects. That’s not a small number. That’s most of your friends, coworkers, or family members who are quietly suffering. It includes:- Lower sex drive
- Delayed or absent orgasm
- Difficulty getting or keeping an erection
- Reduced genital sensation
Severe Side Effects: When to Call Your Doctor
Most side effects fade. But some don’t. And they need immediate attention. Serotonin syndrome is rare but dangerous. It happens when serotonin builds up too high-usually because you’re mixing SSRIs with other drugs like tramadol, MDMA, or even St. John’s Wort. Symptoms start with sweating, shivering, fast heartbeat. Then come confusion, muscle rigidity, high fever. Left untreated, it can kill. If you feel this, go to the ER. Hyponatremia is another hidden risk. It’s when your blood sodium drops too low. Elderly patients are most at risk. Signs: nausea, confusion, headaches, seizures. It’s more common with SSRIs than any other antidepressant. Your doctor should check your sodium levels after 2-4 weeks, especially if you’re over 65. Extrapyramidal symptoms are movement disorders. Akathisia-a feeling of being unable to sit still-is the most common. You pace, fidget, feel restless inside. Dystonia causes painful muscle spasms. Parkinsonism mimics tremors and stiffness. These are often mistaken for anxiety or worsening depression. But they’re drug-induced. Stopping or switching the SSRI usually fixes it. Discontinuation syndrome hits hard if you quit cold turkey. Especially with paroxetine or fluvoxamine-they leave your system fast. You get dizziness, electric-shock sensations in your head, nausea, anxiety, insomnia. It starts within days. The fix? Taper slowly. Reduce your dose by no more than 10-25% every 2-4 weeks. Don’t guess. Work with your prescriber.Why Some SSRIs Are Easier Than Others
Not all SSRIs are the same. Their side effect profiles vary.- Citalopram: Best tolerated overall. Least likely to cause weight gain or sexual issues.
- Escitalopram: Similar to citalopram, but higher risk of dizziness and memory fog.
- Sertraline: Most prescribed in the U.S. Good for anxiety. Lower weight gain risk than paroxetine.
- Fluoxetine: Long half-life. Less withdrawal risk. But higher chance of insomnia and weight gain.
- Paroxetine: Worst for sexual side effects and weight gain. Highest discontinuation rate.
- Fluvoxamine: Highest nausea risk. Often avoided unless for OCD.
What’s New in 2025?
The FDA updated SSRI labels in June 2023 to warn about long-term metabolic risks. Studies now show a 24% higher chance of developing insulin resistance or type 2 diabetes after two years on SSRIs. That’s not just about weight-it’s about how your body processes sugar. New research from Nature Medicine found genetic markers linked to sexual side effects. Soon, blood tests might tell you if you’re genetically prone to them before you even start. That’s precision psychiatry. Pharmaceutical companies are testing next-gen SSRIs. One, Lu AF35700, is in Phase III trials. Early results show 37% fewer sexual side effects. It could be available by 2027.
How to Manage Side Effects Without Quitting
You don’t have to suffer. Here’s what works:- Nausea? Take the pill with food. Try ginger tea. Avoid spicy meals.
- Insomnia? Take it in the morning. Avoid caffeine after noon.
- Drowsiness? Move your dose to nighttime if it helps sleep.
- Sexual issues? Talk to your doctor about bupropion or sildenafil. Don’t suffer in silence.
- Weight gain? Start walking 30 minutes a day. Add protein to every meal.
- Discontinuation? Never stop cold turkey. Plan your taper with your doctor.
When to Consider Stopping
It’s okay to stop if the side effects outweigh the benefits. About 31% of people quit their first SSRI within three months-mostly because of side effects, not lack of results. Signs it’s time to switch:- Sexual dysfunction lasts longer than 6 months
- Weight gain exceeds 5% of your body weight
- You develop movement problems or extreme restlessness
- Your anxiety gets worse instead of better
- You feel worse after 8-12 weeks
Final Thought: Side Effects Are Part of the Treatment
SSRIs changed mental health care. They saved lives. But they’re not harmless. The goal isn’t to avoid side effects entirely-it’s to manage them so they don’t derail your recovery. The best outcome isn’t just feeling better. It’s feeling better and living well.Start the conversation with your doctor before you even fill the prescription. Ask: “What side effects should I expect? Which ones are dangerous? What can I do if they happen?” That’s how you take control.
Do SSRI side effects go away on their own?
Yes, many do. Nausea, headaches, dizziness, and sleep issues usually fade within 2 to 6 weeks as your body adjusts. But sexual dysfunction and weight gain often persist. If side effects last longer than 8 weeks or get worse, talk to your doctor-you may need a dose change or a different medication.
Can SSRIs cause permanent side effects?
In rare cases, yes. Some people report persistent sexual dysfunction even after stopping SSRIs-a condition called PSSD (Post-SSRI Sexual Dysfunction). It’s not fully understood, but case reports suggest it can last months or years. Movement disorders like tardive dyskinesia are also possible with long-term use. These are uncommon, but real. Always report unusual symptoms early.
Which SSRI has the least side effects?
Citalopram is generally the best-tolerated SSRI, with lower rates of weight gain, sexual dysfunction, and discontinuation symptoms. Escitalopram is similar. Sertraline is also well-tolerated and widely used. Paroxetine and fluvoxamine tend to cause the most side effects and are usually avoided unless necessary.
Why do SSRIs make me feel worse at first?
When SSRIs increase serotonin levels, your brain needs time to adapt. In the first 1-2 weeks, this surge can overstimulate certain receptors, causing anxiety, agitation, or nausea. This is temporary. Most people feel better after 3-4 weeks. If you feel severely worse-like suicidal thoughts or panic attacks-contact your doctor immediately.
Is it safe to take SSRIs long-term?
Yes, for many people. SSRIs are safe for years if monitored. But long-term use increases risks like weight gain, insulin resistance, and bone density loss. Regular checkups for blood sugar, weight, and bone health are recommended. Never stop abruptly. Work with your doctor to plan a safe taper if you decide to discontinue.

Richard Eite
December 9, 2025 AT 01:15Jennifer Blandford
December 9, 2025 AT 04:25Katherine Rodgers
December 9, 2025 AT 14:13Olivia Portier
December 9, 2025 AT 19:42Delaine Kiara
December 11, 2025 AT 13:29Courtney Black
December 13, 2025 AT 01:57Ruth Witte
December 13, 2025 AT 04:38Noah Raines
December 13, 2025 AT 19:25Asset Finance Komrade
December 15, 2025 AT 13:34Iris Carmen
December 16, 2025 AT 11:40Gilbert Lacasandile
December 17, 2025 AT 13:48