When you’re tossing and turning every night, waking up exhausted even after eight hours in bed, it’s easy to blame stress or aging. But what if your body is struggling with something deeper-something only a sleep study can uncover? That’s where polysomnography comes in. It’s not just another medical test. It’s the most detailed window into your sleep that medicine has ever created.
What Exactly Is a Polysomnography?
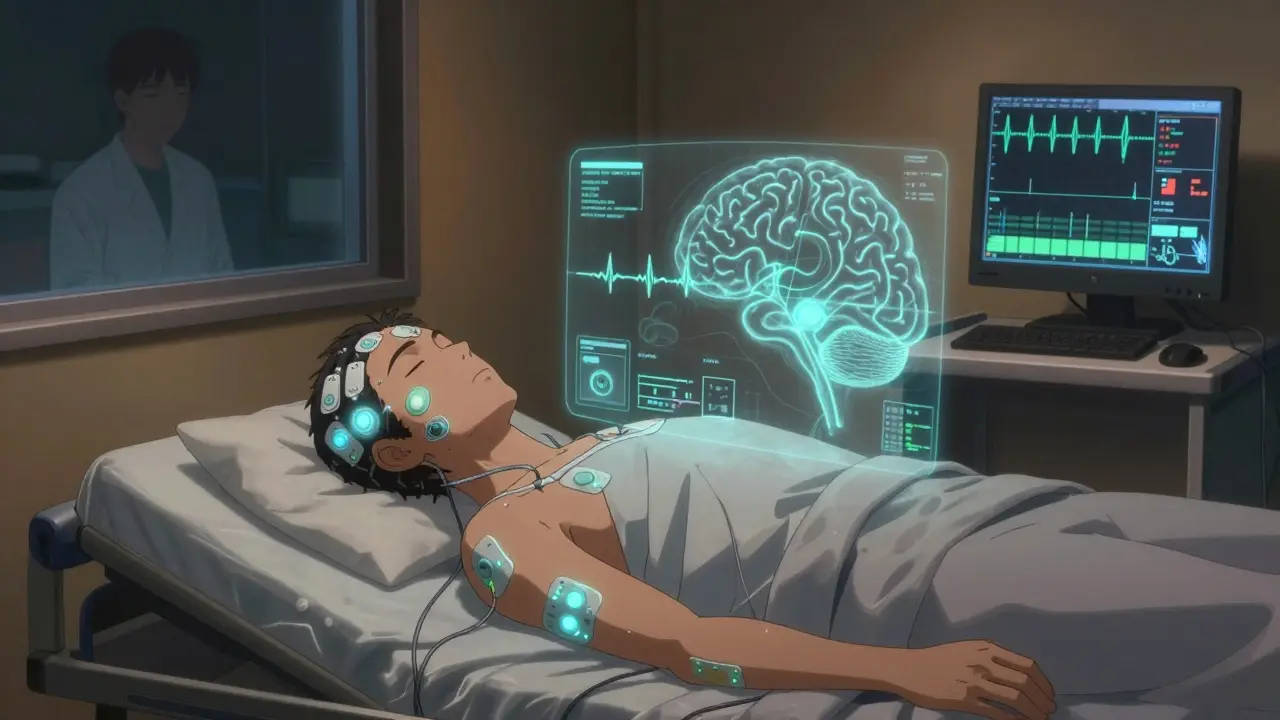
Polysomnography, or PSG, is a full-night sleep study that records up to 16 different body functions while you sleep. The word itself breaks down to “poly” (many), “somno” (sleep), and “graphy” (recording)-so it’s literally a multi-parameter sleep recording. Unlike home sleep tests that only check your breathing, polysomnography watches your brain, eyes, muscles, heart, and breathing all at once. This lets doctors see not just if you stop breathing, but when you stop breathing, how your brain reacts, and whether your sleep stages are normal. It’s the gold standard for diagnosing more than just sleep apnea. Narcolepsy, restless legs syndrome, parasomnias like sleepwalking or night terrors, and even seizures that happen only during sleep-all of these show up clearly on a polysomnography. The American Academy of Sleep Medicine says you need this full test if your symptoms go beyond simple snoring or daytime tiredness. If you’re having unexplained fatigue, sudden muscle weakness, or strange behaviors during sleep, this is the test that gives answers.What Happens During the Study?
You’ll arrive at a sleep center-usually a quiet, hotel-like room with a comfortable bed-about an hour before your normal bedtime. A sleep technologist will attach sensors to your scalp, face, chest, legs, and fingers. Don’t worry: it’s not painful. It’s like sticking small stickers on your skin. There are about 22 sensors total, including:- Electrodes on your scalp to track brain waves (EEG)
- Small patches near your eyes to record eye movements (EOG)
- Straps around your chest and belly to measure breathing effort
- A sensor under your nose to detect airflow
- A clip on your finger to monitor blood oxygen levels
- Electrodes on your chin and legs to check muscle activity
- A tiny camera and microphone to record sounds and movements
What Do the Results Show?
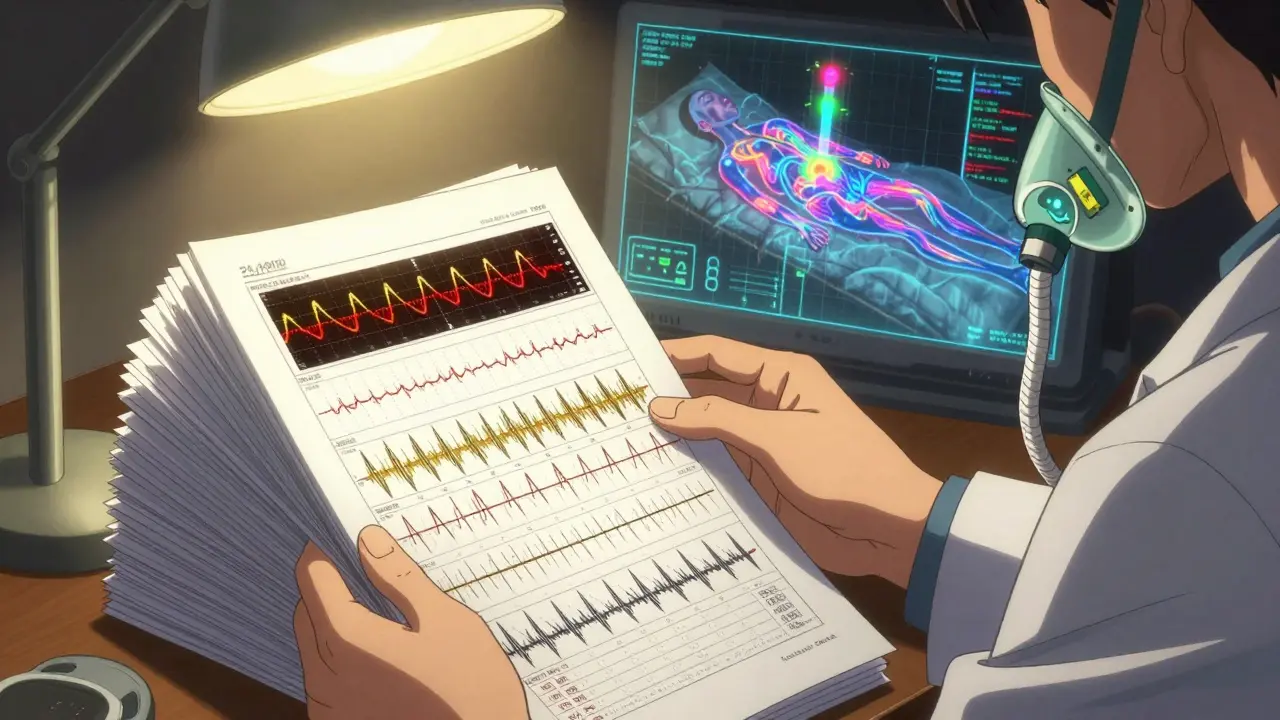
After the night ends, a board-certified sleep doctor spends 2-3 hours analyzing the data. The raw output is over 1,000 pages of numbers and waveforms. Here’s what they’re looking for:- Sleep stages: Did you go through the normal cycle of light sleep, deep sleep, and REM sleep? People with narcolepsy jump straight into REM. Others never get enough deep sleep.
- Apneas and hypopneas: How many times did you stop breathing or breathe too shallowly? If it’s more than 5 per hour, you might have sleep apnea.
- Oxygen drops: Did your blood oxygen fall below 90%? Frequent drops mean your body is under stress.
- Limb movements: Are your legs jerking every 20-40 seconds? That’s restless legs or periodic limb movement disorder.
- Heart rhythm: Any irregular beats during sleep? Sleep apnea can trigger arrhythmias.
- Snoring and behaviors: Was there screaming, punching, or getting out of bed? These point to parasomnias.
How Is It Different From Home Sleep Tests?
Home sleep tests are cheaper and easier-but they’re not the same thing. They usually only monitor airflow, oxygen levels, breathing effort, and heart rate. That’s enough for a straightforward case of obstructive sleep apnea in someone who’s overweight and snores loudly. But if you have other symptoms-like falling asleep during the day, sudden muscle weakness, or weird movements at night-a home test will miss it. In fact, about 15-20% of home tests fail because the device falls off or the patient doesn’t use it right. In-lab polysomnography fails less than 5% of the time. And unlike home tests, polysomnography can diagnose narcolepsy, REM sleep behavior disorder, or nocturnal seizures-conditions that require brain wave monitoring.What Is a Split-Night Study?
If your sleep study shows severe sleep apnea early in the night-say, more than 30 breathing pauses per hour-the sleep doctor might decide to do a split-night study. That means after the first 2-3 hours of diagnostic monitoring, they’ll wake you up, fit you with a CPAP mask, and adjust the air pressure while you sleep the rest of the night. This saves you a second visit. About 35% of polysomnography studies in the U.S. now include CPAP titration. It’s not for everyone-only if the apnea is clearly severe and the patient can tolerate the mask. But for those who qualify, it cuts the time to treatment in half.What Should You Do Before the Test?
You don’t need to fast or change your diet. But you should:- Avoid caffeine after noon the day before
- Don’t nap during the day
- Stick to your usual bedtime routine
- Wash your hair without conditioner-it helps sensors stick better
- Bring your own pillow, pajamas, and anything that helps you sleep
Who Covers the Cost?
Medicare covers 80% of the cost if your doctor documents symptoms like loud snoring, witnessed breathing pauses, or excessive daytime sleepiness. Private insurers usually require prior authorization. Most will cover polysomnography if you’ve tried a home test first and it was inconclusive-or if your symptoms suggest something more complex than simple sleep apnea. In the U.S., about 1.5 million in-lab sleep studies are done each year. That number is growing by 8% annually as more people realize sleep isn’t just about quantity-it’s about quality.What Happens After the Results?
Your sleep doctor will schedule a follow-up to explain the findings. If you have sleep apnea, you’ll likely be prescribed CPAP therapy. If it’s narcolepsy, you might get stimulants or sodium oxybate. Restless legs? Medications like ropinirole. Parasomnias? Safety measures and sometimes low-dose antidepressants. The goal isn’t just to give you a label. It’s to fix your nights so you wake up refreshed, think clearly, and avoid long-term risks like high blood pressure, heart disease, or stroke.Are There Downsides?
Some people worry about sleeping with wires. Others feel self-conscious. A few can’t fall asleep at all the first night-this is called the “first night effect.” It’s normal. The data from the second night is often more accurate, but even the first night usually gives enough info to make a diagnosis. Newer wireless systems are cutting down the number of wires from 20 to just 5 or 7. That’s making it easier to move around and sleep more naturally. Some centers now use soft, fabric-based sensors instead of hard electrodes. Comfort is improving. Still, nothing beats the full picture you get from an in-lab study. Home tests are useful for simple cases. But if your sleep problems are complex-if you’re not just tired, but confused, unsteady, or acting out dreams-you need the full polysomnography.Is a polysomnography painful?
No, it’s not painful. Sensors are attached with adhesive or soft bands. You might feel slight pressure from the chest belts or a small clip on your finger, but nothing invasive. Most people say the discomfort is less than a routine blood draw.
Can I sleep with all those sensors on?
Yes, most people do. The sleep center is designed to feel like a hotel room-quiet, dark, and private. Technologists are trained to help you relax. Even if you don’t sleep as well as you do at home, you usually get enough data for an accurate diagnosis. About 85% of patients complete the study successfully.
How long until I get my results?
It usually takes 1-2 weeks. The sleep technologist collects the data the night of the study, but a board-certified sleep physician must manually review over 1,000 pages of recordings. This takes several hours per patient. Rushed results aren’t reliable, so patience is part of the process.
Do I need to stay overnight?
Yes. Polysomnography requires monitoring your full sleep cycle, which includes multiple transitions between REM and non-REM stages. These cycles repeat every 90 minutes and typically occur 4-6 times per night. A partial night or daytime test won’t capture the full picture.
Can polysomnography diagnose insomnia?
Not directly. Insomnia is diagnosed mainly through sleep diaries and questionnaires. But polysomnography can rule out other conditions that mimic insomnia-like sleep apnea, periodic limb movement disorder, or circadian rhythm disorders. If your sleep study shows normal sleep architecture, your doctor may suspect primary insomnia and recommend cognitive behavioral therapy instead.
Are there alternatives to in-lab polysomnography?
Home sleep apnea tests (HSAT) are the main alternative-but they only screen for obstructive sleep apnea. They can’t detect narcolepsy, parasomnias, or central sleep apnea. If your symptoms are complex, your doctor will still require an in-lab study. HSAT is only appropriate for straightforward cases with high suspicion of obstructive sleep apnea.

Christina Bischof
December 15, 2025 AT 07:07Lisa Davies
December 17, 2025 AT 05:50Nupur Vimal
December 18, 2025 AT 19:50Cassie Henriques
December 20, 2025 AT 17:53Jake Sinatra
December 20, 2025 AT 18:03Michelle M
December 22, 2025 AT 11:01Benjamin Glover
December 24, 2025 AT 06:14Raj Kumar
December 24, 2025 AT 18:37Melissa Taylor
December 25, 2025 AT 19:42John Brown
December 26, 2025 AT 18:37Jocelyn Lachapelle
December 28, 2025 AT 03:01