When pain becomes a daily companion, pills aren’t the only answer-and often, they’re not the best one. Many people turn to medication because it’s quick, but what if you could reduce pain by moving differently? Physical therapy for pain isn’t about pushing through discomfort. It’s about retraining your body to move without triggering pain signals. And the science backs it up: structured exercise, smart stretching, and gradual restoration can cut chronic pain by half in just a few weeks.
How Movement Actually Stops Pain
Pain isn’t just a signal from your muscles or joints. It’s a complex response from your nervous system. When you move in a controlled, consistent way, your brain starts to reinterpret those signals. Exercise releases endorphins-your body’s natural painkillers. But more than that, it rewires how your nerves talk to your brain. Studies show that 65-75% of your maximum heart rate for 20 minutes or more triggers something called exercise-induced hypoalgesia. That’s a fancy way of saying: movement literally dulls pain.
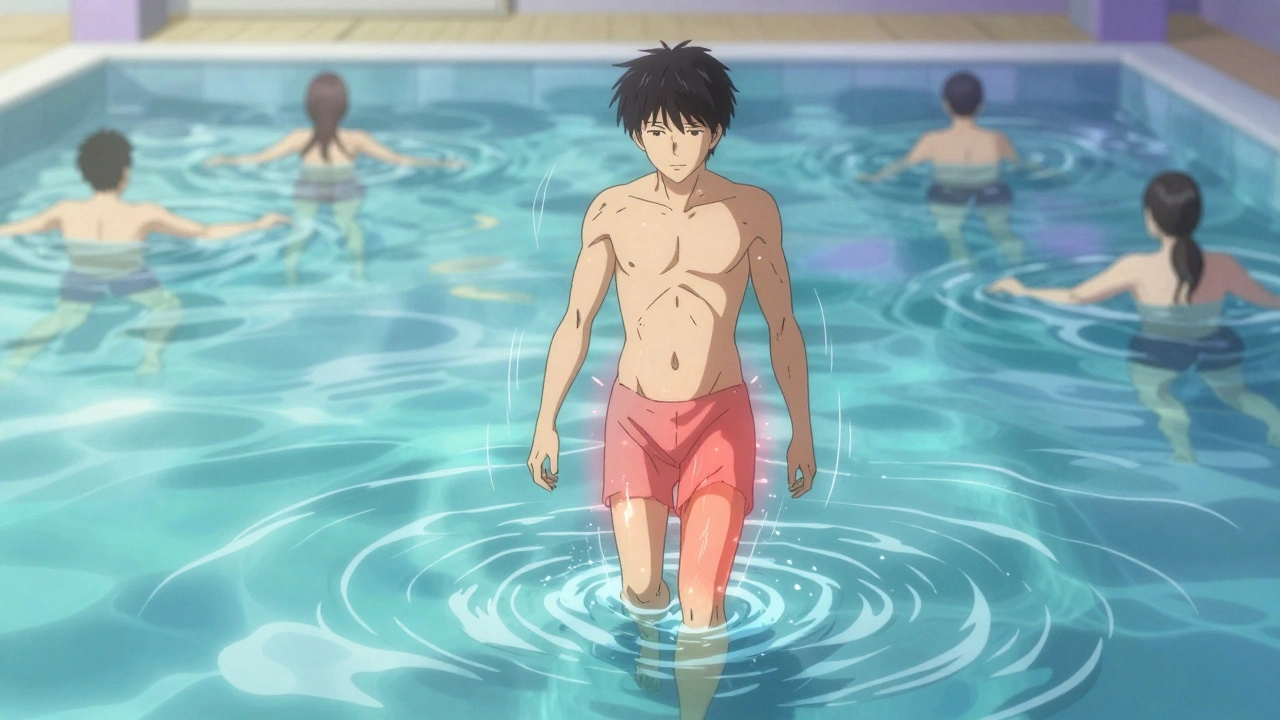
It’s not about working out until you’re exhausted. It’s about consistency. A 2023 Mayo Clinic study found that water walking reduced knee joint stress by 50% compared to land walking. For someone with osteoarthritis, that means less pain during the workout-and less pain afterward. Even walking 15 minutes a day, five times a week, can lead to measurable drops in pain scores within four weeks.
The Right Kind of Exercise for Your Pain
Not all exercises are created equal when it comes to pain. High-intensity workouts can actually make things worse for some conditions. If you have fibromyalgia, pushing past 80% of your max heart rate increases pain in over 20% of cases, according to a 2020 review. But moderate activity? That’s where the magic happens.
- Walking: Start with 10 minutes a day. Add 2-3 minutes every few days. Use supportive shoes. If your pain spikes above 3 out of 10 during the walk, slow down-not stop.
- Swimming or water aerobics: The water supports your weight. This is ideal for back pain, hip arthritis, or anyone who finds land movement too jarring.
- Cycling (stationary or outdoor): Low impact, easy to control intensity. Adjust the resistance so you can talk but not sing.
- Tai chi: For fibromyalgia and chronic neck pain, this slow, flowing practice has been shown to reduce pain 30% more than regular aerobic exercise after 12 weeks.
- Resistance bands: You don’t need weights. A simple loop band can strengthen glutes, shoulders, and back muscles. Two minutes a day, three times a week, can cut shoulder pain by nearly 30%.
One of the most surprising findings? Short bursts work. A Duke University study of office workers found that two minutes of neck and shoulder exercises-done three times a day-gave the same pain relief as a full 12-minute routine. You don’t need hours. You need consistency.
Stretching: Not Just for Flexibility
Stretching isn’t about touching your toes. It’s about releasing tension that’s been locked in by pain. When you hurt, your muscles tighten up to protect you. But that protection becomes a trap. Static stretching-holding a position without bouncing-helps reset that tension.
Here’s what works:
- Hold each stretch for 30 to 60 seconds. Repeat 2-3 times per muscle group.
- Do it 5-7 days a week. Even on days you feel stiff.
- Focus on areas linked to your pain: hamstrings for lower back, chest for neck, hips for knee pain.
A 2023 clinical report from Delmarva Physical Therapy showed that people who stretched daily improved their range of motion by 15 to 25 degrees in just four weeks. That might not sound like much, but for someone who couldn’t bend to tie their shoes, it’s life-changing.
And breathing matters. Many people hold their breath when they stretch. That keeps muscles tight. Try this: inhale through your nose, exhale slowly through your mouth as you ease into the stretch. Let the air out, and let the tension go.

Restoration: Getting Back to What You Love
Pain doesn’t just hurt-it steals your life. You stop lifting groceries. You avoid stairs. You skip walks with friends. Physical therapy isn’t just about reducing pain numbers. It’s about restoring function.
That means relearning how to move safely. A 2024 Physiopedia guideline says to increase activity by only 10-15% per week. If you walked 15 minutes last week, aim for 17 this week. If you did 10 squats, try 11. Small steps prevent setbacks.
The 2-hour pain rule is key: if your pain goes back to normal within two hours after exercise, you’re on the right track. If it lingers longer or gets worse, you pushed too hard. Adjust. Don’t quit.
People with chronic back pain often benefit from targeted core and glute strengthening. Dr. James Fricton from UT Health Austin says 70% of patients with long-term back pain see major improvement when they stick to a simple home program that includes bridges, bird-dogs, and planks-done correctly.
What Doesn’t Work-and Why
Not every therapist knows the latest science. A 2024 survey found that 68% of physical therapists feel undertrained in prescribing aerobic or resistance exercise for pain. That means some people get generic advice: “Just move more.” But that’s not enough.
Bad technique makes pain worse. Reddit user u/BackPainSufferer shared that straight leg raises cut his sciatica pain from 7/10 to 2/10 in three weeks. But another user said the same exercise made his pain explode because he was arching his back instead of keeping it neutral.
Here’s the reality: if you’re doing an exercise and it hurts more than 3/10 during the movement, or if pain doesn’t return to baseline within an hour, you’re doing it wrong. Ask for feedback. Watch a video. Get a second opinion.
And don’t believe the myth that “exercise alone can fix everything.” Dr. Jane Smith of Advanced Pain Medical points out that 35% of patients need more than movement-maybe manual therapy, posture correction, or stress management. Physical therapy is powerful, but it’s not always the only tool.
How to Start Today
You don’t need a gym. You don’t need a prescription. You just need to begin.
- Choose one movement: Walk, swim, or use a resistance band for 5 minutes today.
- Stretch two areas: Hamstrings and shoulders. Hold each for 45 seconds. Breathe out slowly.
- Track your pain: Use a 0-10 scale. Write it down after each session.
- Stick to the 2-hour rule: If pain returns to normal within two hours, keep going.
- Gradually increase: Add one minute to your walk, one more rep to your band exercise, every few days.
Most clinics offer a free 15-minute consultation. Ask if they use evidence-based protocols. Look for therapists who mention VO2 max, progressive overload, or the Numeric Pain Rating Scale. If they just say “we’ll see how you feel,” keep looking.
The Arthritis Foundation’s two-minute exercise routine has helped over 1,200 people reduce neck and shoulder pain by 31% in four weeks. You can find it online-no appointment needed. Try it before you buy a new pillow or order another pain patch.
What’s Changing Right Now
Physical therapy is evolving fast. In March 2024, Mayo Clinic released a validated 15-minute back exercise protocol that helped 62% of patients cut their pain in half. The American Physical Therapy Association updated its guidelines in early 2024 to include condition-specific exercise algorithms based on patient feedback.
Telehealth is now part of most programs. Many clinics send video demos via apps. One VA study showed that patients who got video instructions were 78% more likely to stick with their home program than those who only got paper handouts.
And the trend is clear: healthcare systems are pushing physical therapy as a first-line treatment. The American College of Physicians now says to try exercise and manual therapy before any pain meds for back pain. Medicare covers 80% of sessions for approved conditions. This isn’t a fringe option anymore-it’s mainstream.
With over $58 billion spent globally on non-drug pain relief in 2023, physical therapy is the fastest-growing piece of that pie. And it’s growing because it works-for real people, in real lives.
Can physical therapy help with chronic pain without medication?
Yes. Multiple studies show that structured exercise and stretching reduce chronic pain by 50-75% in 6-8 weeks for conditions like osteoarthritis, fibromyalgia, and lower back pain. It works by changing how your nervous system processes pain signals, not just masking symptoms. Many patients stop needing painkillers after 3-4 months of consistent therapy.
How long until I feel less pain from physical therapy?
Most people notice small improvements within 2-3 weeks. Pain scores often drop by 20-30% in the first month. Significant relief-like being able to walk without limping or sleep through the night-usually happens between 6 and 10 weeks. The key is sticking with it. Skipping days slows progress.
Is it normal for pain to get worse at first?
Mild soreness is normal, especially if you haven’t moved much in a while. But sharp, shooting, or worsening pain isn’t. Use the 2-hour rule: if pain returns to your baseline within two hours after exercise, it’s safe to continue. If it lasts longer or gets worse, you may be doing too much or using wrong form. Adjust or ask for help.
Do I need a referral to see a physical therapist?
In the UK and many US states, you can see a physical therapist directly without a doctor’s referral. Medicare and most private insurers cover physical therapy for pain without a referral if it’s medically necessary. Always check your plan, but don’t wait for paperwork if you’re in pain. Many clinics offer free screenings.
What if I can’t afford physical therapy?
You don’t need expensive sessions to benefit. Free resources like the Arthritis Foundation’s two-minute exercises, YouTube channels from accredited clinics (like Mayo Clinic or Johns Hopkins), and community center classes can give you everything you need. Focus on consistency over cost. Ten minutes a day, done right, beats one expensive session you never repeat.
How often should I do physical therapy exercises at home?
Aim for daily movement-even if it’s just 5-10 minutes. Stretching should be done 5-7 days a week. Strength and aerobic exercises can be done 3-5 days a week. The goal is to build habit, not intensity. Missing a day? Just get back on track the next day. Progress isn’t linear.

Yasmine Hajar
December 6, 2025 AT 03:08I tried this for my lower back and holy crap it actually worked. Started with 10 minutes of walking and hamstring stretches - didn’t believe it at first, but after three weeks I can bend over to tie my shoes without groaning. No pills. No injections. Just movement. Mind blown.
Also, the 2-hour rule? Life-changing. I used to quit whenever it hurt. Now I just chill if it lingers past two hours. Genius.
Karl Barrett
December 6, 2025 AT 17:38It’s fascinating how neuroplasticity underpins this entire paradigm shift. The nociceptive pathways aren’t static - they’re dynamically modulated through proprioceptive feedback loops and endogenous opioid release. What we’re seeing here isn’t merely symptom suppression, it’s central sensitization reversal via graded motor imagery and aerobic threshold modulation.
That said, the 65-75% HR zone is critical. Below that, you get negligible hypoalgesic effects. Above? Sympathetic overdrive triggers glutamate spillover - counterproductive. The Mayo water-walking data is robust, but it’s the Delmarva stretching metrics that really validate the cortical reorganization hypothesis.
Jake Deeds
December 8, 2025 AT 15:16Ugh. I’m so tired of people treating physical therapy like some magical wellness hack. I’ve been to three different PTs who told me to ‘just move more’ - and guess what? I ended up with a torn meniscus because I listened to some random Reddit post instead of a real doctor.
Not everyone has the luxury of ‘consistency.’ Some of us have jobs that leave us exhausted. Some of us have insurance that won’t cover anything. And some of us just need a damn pill to function.
Stop glorifying movement like it’s the only moral path. Pain isn’t a character flaw.
val kendra
December 8, 2025 AT 19:47Just started the two-minute neck exercises from the Arthritis Foundation. Did them at my desk during Zoom calls. Didn’t think it’d do anything. Now my shoulders don’t scream at me by 11am. Seriously. Five minutes a day. No equipment. Just breathe out as you stretch.
Also - stop doing straight leg raises if your back arches. I did that for months and made my sciatica worse. Found a YouTube video from Johns Hopkins that showed how to brace your core. Game changer. Don’t wing it. Watch the form.
And yeah, you don’t need a referral. Just call a clinic and ask if they do ‘direct access.’ Most do. No shame in asking.
Consistency > intensity. Always.
Isabelle Bujold
December 10, 2025 AT 06:59As someone who’s been managing fibromyalgia for over a decade, I can say with absolute certainty that movement, when done with intention, is the single most effective tool I’ve ever encountered - far surpassing any medication, supplement, or alternative therapy I’ve tried. The key, as the article notes, is not pushing through pain but working within the window of tolerable discomfort - what I call the ‘sweet spot of sustainable effort.’
For me, tai chi was the turning point. Not because it’s ‘gentle,’ but because it taught me to move with awareness rather than force. The 30% reduction in pain after 12 weeks wasn’t just statistical - it was emotional. I started sleeping again. I stopped canceling plans. I stopped feeling like a burden.
And yes, breathing matters. I used to hold my breath during stretches like I was preparing for a sprint. Now I exhale like I’m blowing out birthday candles - slow, deliberate, releasing tension with every breath. It’s not magic. It’s neuroscience. And it’s accessible to anyone willing to show up, even for five minutes.
Don’t let the noise of ‘just move more’ undermine the precision this requires. It’s not about quantity. It’s about quality of attention.
George Graham
December 12, 2025 AT 03:04My mom had chronic knee pain for years. She tried everything - injections, creams, even acupuncture. Nothing stuck. Then she started water walking three times a week. No fancy gear. Just a pool and 20 minutes. Within six weeks, she was gardening again. No pain meds.
She didn’t even know what ‘exercise-induced hypoalgesia’ meant. She just knew it felt better. And that’s the point. You don’t need to understand the science to benefit from it.
Start small. Stay consistent. Celebrate the tiny wins. Walking to the mailbox without wincing? That’s a victory.
And if you’re feeling discouraged? You’re not alone. But you’re closer than you think.
John Filby
December 13, 2025 AT 05:46Just tried the resistance band glute bridges last night. 10 reps. Felt it in my hips. Pain was at 6/10 before. Now it’s 3/10 after 2 hours. 😊
Also, the breathing thing? I didn’t realize I was holding my breath during stretches. Now I’m like… inhale… exhale like I’m fogging up a mirror… it’s weirdly calming.
Anyone else do these with their dog watching like they’re the coach? Mine just stares. Judging me. But I love her for it.
Elizabeth Crutchfield
December 14, 2025 AT 02:20omg i did the neck thing and now i can turn my head without it feeling like my spine is breaking 😭 thank you thank you thank you
also i spelled everything wrong but u get the point lol
Ben Choy
December 16, 2025 AT 00:00Just wanted to say - this isn’t just for people with chronic pain. I’m 28 and have desk-job stiffness that felt normal until I started doing these 2-minute resets. Now I feel like a different person. No more ‘I need a nap after lunch’ fatigue.
Also, the 10% weekly increase rule? Huge. I tried jumping to 20 minutes of walking and ended up in bed for two days. Lesson learned. Slow and steady wins the race.
And yes - the VA video thing works. I got a link from my PT app. Watched it twice. Did it right. Pain dropped. 🙌
Emmanuel Peter
December 17, 2025 AT 21:07Let’s be real - most of you are just avoiding real treatment. You think stretching is gonna fix a herniated disc? Please. You’re wasting time. If you’re still in pain after a month of this, you need an MRI, not a yoga video.
And don’t get me started on ‘no referral needed.’ That’s how people end up with permanent nerve damage. You think a YouTube video knows your spinal alignment? No. A real PT does.
Stop romanticizing DIY rehab. This isn’t a TikTok trend. It’s a medical condition. Treat it like one.