Medication Pancreatitis Risk Checker
How This Tool Works
This tool helps you identify if you're taking medications that may increase your risk of drug-induced pancreatitis. Based on clinical evidence, certain medications carry higher risks for this serious condition. Please enter the medications you're currently taking.
If you have persistent upper abdominal pain that radiates to your back, especially after eating, seek immediate medical attention. The difference between life and death can be whether anyone noticed warning signs in time.
When you take a new medication, you expect relief-not a life-threatening emergency. But for some people, common prescriptions can trigger severe pancreatitis, a sudden and dangerous inflammation of the pancreas that kills up to 30% of those who develop it. Unlike gallstones or alcohol, which are the usual suspects, drug-induced pancreatitis flies under the radar. It doesn’t come with obvious red flags. Symptoms creep in slowly. Doctors often miss it. And by the time it’s caught, the damage can be irreversible.
What Does Severe Pancreatitis from Medications Actually Look Like?
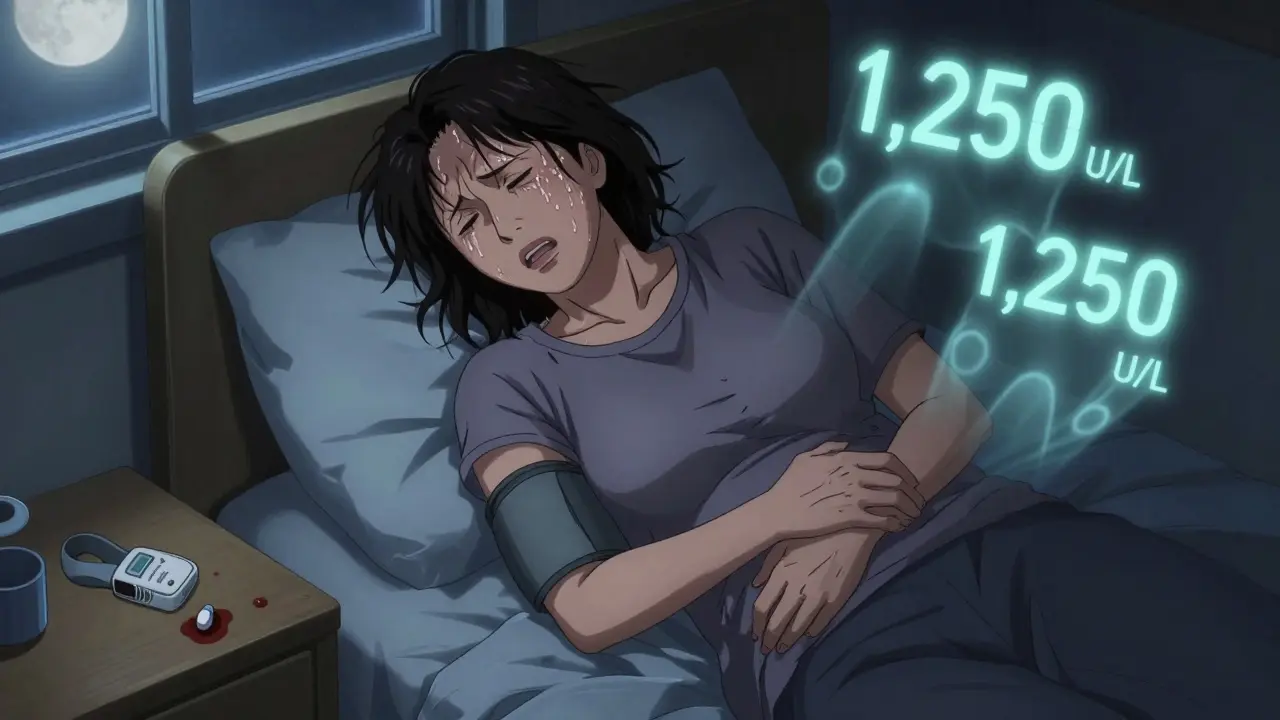
Most people think of pancreatitis as sudden, sharp pain in the upper belly that radiates to the back. That’s true-but with drug-induced cases, the timeline is different. You might have been on the medication for weeks or even months. A 45-year-old woman in Bristol took lisinopril for high blood pressure for six months before waking up at 3 a.m. with pain so bad she couldn’t breathe. Her lipase level hit 1,250 U/L-over 20 times the normal limit. She spent five days in the hospital. No gallstones. No alcohol use. Just a common blood pressure pill.
That’s the pattern. The pain isn’t always sudden. It might start as mild discomfort after meals, then worsen over days. Nausea, vomiting, fever, and a rapid heartbeat often follow. In severe cases, you’ll see signs of organ failure: low blood pressure, trouble breathing, or confusion. These aren’t just bad stomach bugs. They’re warning signs your pancreas is dying.
Doctors rely on three things to confirm it: elevated lipase (not amylase-it’s more specific), imaging showing swelling or dead tissue in the pancreas, and ruling out other causes like gallstones or alcohol. If you’re on any of the high-risk drugs listed below and have persistent upper abdominal pain, ask for a lipase test. Don’t wait. Delaying diagnosis increases your risk of complications by 37%.
Which Medications Are Most Likely to Cause This?
Not all drugs carry the same risk. Eight classes stand out based on decades of clinical data and recent FDA alerts:
- ACE inhibitors like lisinopril and enalapril-commonly prescribed for blood pressure and heart failure
- Diuretics such as furosemide and hydrochlorothiazide-used for fluid retention
- Statins like simvastatin and atorvastatin-for cholesterol
- Antidiabetic drugs including exenatide (Byetta), sitagliptin (Januvia), and SGLT2 inhibitors like canagliflozin
- Immunosuppressants such as azathioprine and valproic acid-used for autoimmune diseases and epilepsy
- Oral contraceptives containing ethinyl estradiol
- Antiretrovirals like didanosine (rare now but still documented)
Valproic acid and azathioprine are especially dangerous. One study found 22% of people on valproic acid developed necrotizing pancreatitis-meaning parts of the pancreas started dying. Azathioprine users had an 18% risk. These aren’t rare outliers. They’re predictable outcomes in high-risk groups.
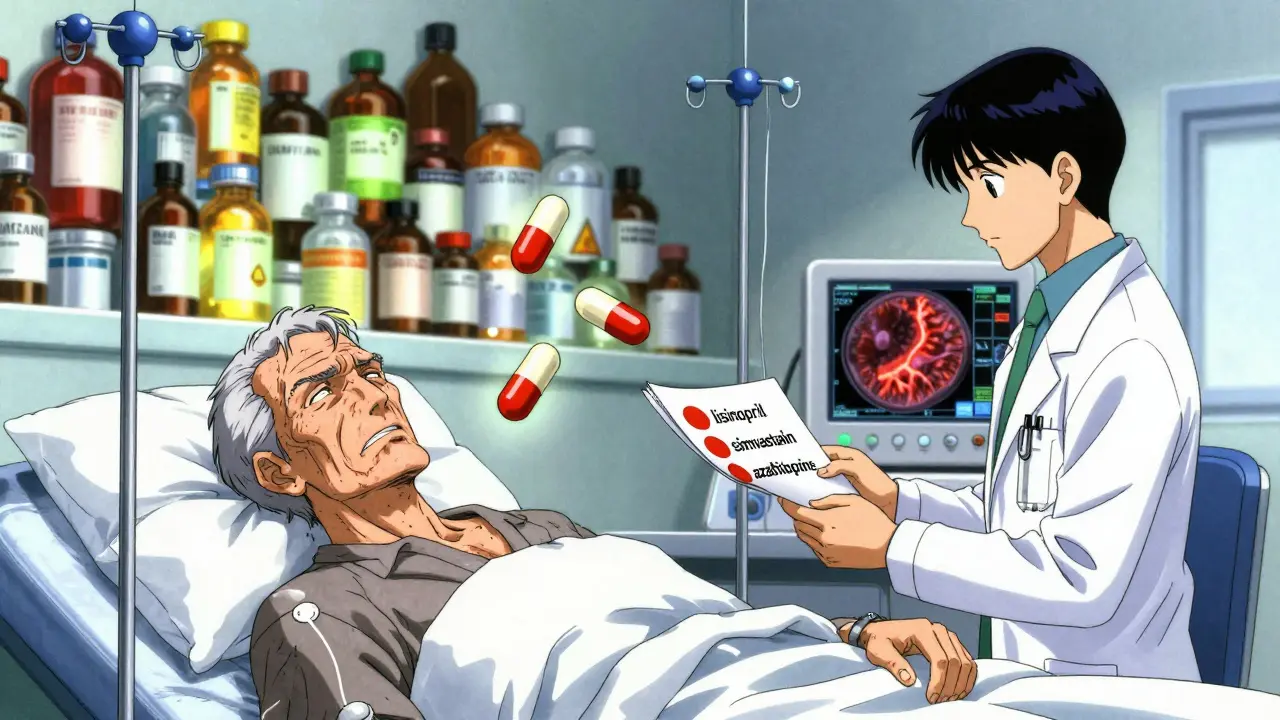
What’s worse? Many people are on multiple high-risk drugs. A 72-year-old with hypertension, high cholesterol, and Crohn’s disease might be taking lisinopril, simvastatin, and azathioprine-all at once. That’s not just polypharmacy. That’s a ticking time bomb. The average patient with drug-induced pancreatitis takes 5.2 medications. Compare that to 2.7 for others. The more pills you take, the higher the chance one of them is harming your pancreas.
Why Is This So Hard to Diagnose?
Because the symptoms look like everything else. Gastritis. Gallbladder flare-up. Kidney stones. Even food poisoning. That’s why 68% of patients on Drugs.com and PatientsLikeMe reported delayed diagnosis. One Reddit user, a physician, wrote about a 62-year-old on simvastatin for three years who suddenly developed lipase levels of 2,800. His doctor dismissed it as indigestion for two days. By the time they acted, he was in critical condition.
Doctors aren’t trained to think “medication” first. They look for gallstones, alcohol, or genetics. But drug-induced pancreatitis doesn’t leave a footprint like those do. There’s no scar tissue from years of drinking. No bile duct blockage. Just a sudden, unexplained explosion of inflammation. And because the reaction can happen weeks after starting the drug, it’s easy to dismiss.
Even the medical community debates how many cases are real. One expert says up to 40% of reported cases are just coincidence-especially with statins, which millions take. But here’s the problem: if you’re one of the 1.4% to 3.6% of people who react, it doesn’t matter if it’s rare. It matters that you lived through it.
How Is It Treated? The Clock Is Ticking
There’s no magic pill. The only proven cure is stopping the drug-fast. If you wait more than 24 hours after suspicion, your risk of complications spikes by 37%. That’s not a suggestion. It’s a medical imperative.
Once the drug is pulled, treatment is supportive but aggressive:
- IV fluids-250 to 500 mL per hour in the first 24 to 48 hours. This keeps blood flowing to the pancreas. Dehydration makes it worse.
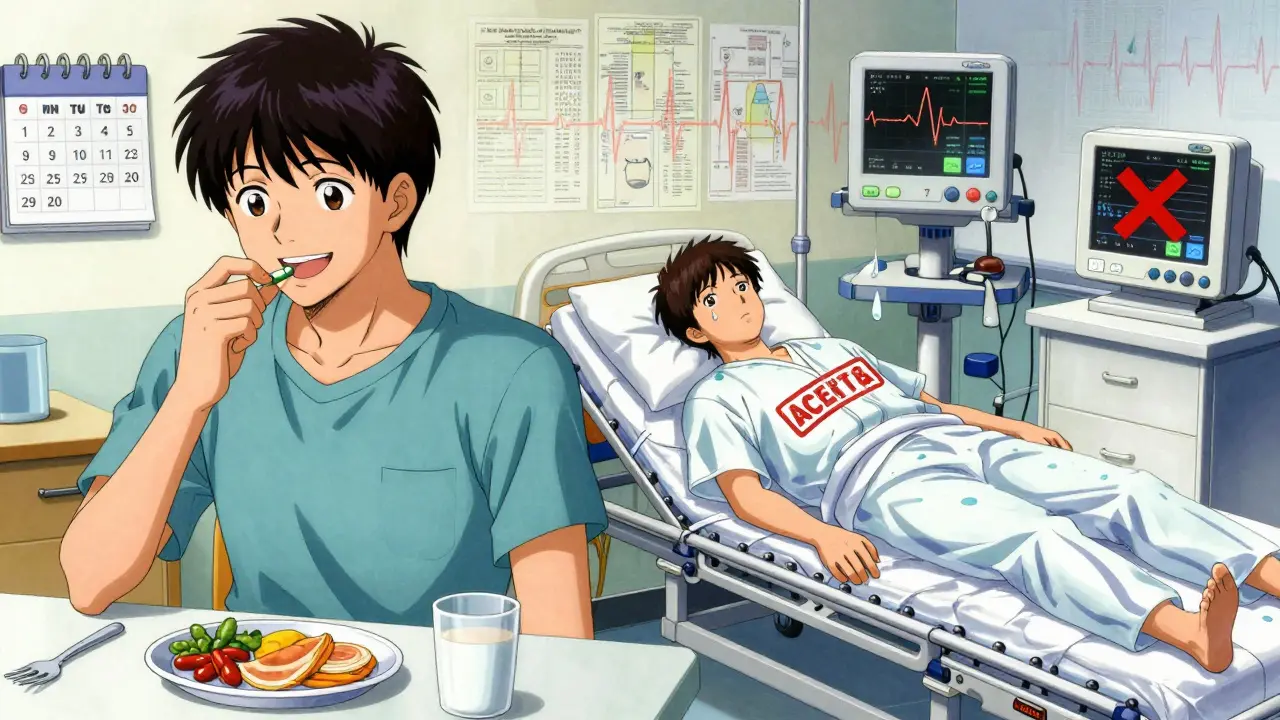
- Pain control-Start with acetaminophen. If that’s not enough, use morphine in small doses. Avoid meperidine-it can worsen spasms.
- Early feeding-You might be told to fast. But if you can’t eat by day two, get a feeding tube placed through your nose into the small intestine. Starving the pancreas doesn’t help. Feeding it gently does.
- Antibiotics-Only if there’s infected dead tissue. Routine use increases resistance and doesn’t help.
Most patients improve within a week if caught early. But if you develop necrosis-dead tissue covering more than 30% of the pancreas-you’re looking at weeks in the ICU. Some need surgery. Others never fully recover.
What Happens After You Recover?
If you survive, you’re not done. You must avoid every drug in the same class. If lisinopril caused it, no other ACE inhibitor is safe. If azathioprine triggered it, you’ll need an alternative for your autoimmune condition. There’s no second chance.
Some patients get rechallenged-meaning they’re given the drug again to confirm it caused the reaction. But this is rare. Ethically, it’s risky. And in 99% of cases, it’s unnecessary. Once you’ve had it, you’re at higher risk for recurrence. Period.
Long-term, your pancreas may heal completely. But you’ll need regular check-ups. Some develop chronic pancreatitis or diabetes later. One study found 12% of survivors had new-onset diabetes within five years.
What Should You Do If You’re on a High-Risk Drug?
You don’t need to panic. But you do need to be alert.
- Know your meds. If you’re on one of the eight high-risk classes, write them down.
- Track any new abdominal pain-especially if it’s persistent, worse after eating, or radiates to your back.
- Ask your doctor for a lipase test if you have unexplained symptoms. Don’t wait for them to suggest it.
- If you have Crohn’s, lupus, epilepsy, or are on multiple medications, make sure your doctor knows the risk.
- Keep a list of all your drugs-including supplements-to show every provider.
And if you’ve had pancreatitis before? Tell every new doctor. Write it in your medical records. Say it out loud: “I had drug-induced pancreatitis. I cannot take ACE inhibitors, statins, or azathioprine again.”
Why This Is Getting Worse
More people are on more drugs. The average American over 65 takes five prescriptions. The FDA received over 4,200 pancreatitis reports linked to medications in 2022-up nearly 13% from the year before. New drugs like SGLT2 inhibitors for diabetes are now carrying black box warnings after dozens of cases were reported. Immunotherapy for cancer is causing pancreatitis in nearly 10% of patients, with over a third progressing to severe forms.
Hospitals are starting to respond. In the U.S., 78% of academic centers now have electronic alerts in their systems that flag high-risk drug combinations. But outside big hospitals? Most clinics still don’t screen. Patients are still being told it’s “just gastritis.”
This isn’t just a medical issue. It’s a system failure. We’ve gotten good at prescribing. We’re terrible at monitoring.
Can you get pancreatitis from over-the-counter meds?
Yes. While most cases come from prescription drugs, some OTC products have been linked. High doses of NSAIDs like ibuprofen or naproxen, especially with long-term use, have caused rare cases. Herbal supplements like green tea extract and kava have also been reported. Always check with your pharmacist before combining new supplements with existing meds.
Is drug-induced pancreatitis permanent?
In most cases, no-if caught early and the drug is stopped. The pancreas can heal completely. But if you develop necrosis or delay treatment, permanent damage can occur. Some people end up with chronic pancreatitis, digestive problems, or diabetes. The key is speed: stopping the drug within 24 hours of suspicion gives you the best shot at full recovery.
Can I ever take the medication again after recovering?
No. Re-exposure carries a very high risk of recurrence, often more severe. Even if you had a mild case, your body has already shown it reacts badly. Doctors will not rechallenge you unless it’s absolutely life-saving and no alternatives exist-which is extremely rare. Avoid all drugs in the same class.
How do I know if my pain is from my meds or something else?
If you’re on a known high-risk drug and have persistent upper abdominal pain-especially if it radiates to your back, worsens after eating, or comes with nausea and fever-get a lipase blood test. Don’t wait for a diagnosis. Ask for it. If your lipase is more than three times the upper limit of normal and other causes (gallstones, alcohol) are ruled out, drug-induced pancreatitis is likely. Timing matters: symptoms usually appear within 4 weeks of starting the drug.
Are there tests to predict if I’m at risk before taking a drug?
Only for one drug: azathioprine. A simple blood test can check your TPMT gene. If you have a variant, your body can’t break down the drug properly, and your risk of pancreatitis jumps 10-fold. For other drugs, no predictive test exists yet. But if you’ve had pancreatitis before, or have a family history, tell your doctor. They may choose safer alternatives.
Final Thought: Your Meds Aren’t Always Safe-Even the Common Ones
Medications save lives. But they can also break you. The same pill that lowers your blood pressure or cholesterol could be quietly attacking your pancreas. You don’t need to stop taking your meds. But you do need to know the signs. Ask questions. Demand tests. Speak up when something feels wrong. Because when it comes to drug-induced pancreatitis, the difference between life and death isn’t always the treatment-it’s whether anyone noticed the warning signs in time.

William Liu
December 18, 2025 AT 22:31This is the kind of post that should be mandatory reading for anyone on prescriptions.
Erica Vest
December 20, 2025 AT 19:39I'm an ER nurse and I've seen this too many times. Patients come in with lipase over 1000, and when we ask about meds, they say 'oh yeah, I've been on that blood pressure pill for a year.' No one connects the dots until it's too late. Always ask about meds first, even if it seems obvious. It's not always gallstones.
Chris porto
December 21, 2025 AT 16:51It's strange how we trust pills like they're harmless. We check food labels for sugar, but we don't question what a drug is doing to our organs. The pancreas doesn't scream. It just stops working. And by then, it's too late. Maybe we need to treat meds like we treat food-know what's in them, know the risks, know when to stop.
Adrienne Dagg
December 22, 2025 AT 00:48My aunt had this after taking simvastatin. She was fine for 18 months. Then one morning, she couldn't stand up. They thought it was a gallbladder attack. Took 3 days to diagnose. She’s lucky she didn’t die. 🙏
mary lizardo
December 22, 2025 AT 18:09It is, of course, entirely unsurprising that pharmaceutical companies have failed to adequately warn the public about the potential for life-threatening adverse reactions to their profit-driven products. The systematic suppression of post-marketing surveillance data is a well-documented ethical failure in modern medicine.
Sajith Shams
December 24, 2025 AT 12:52Statins cause pancreatitis? That’s a joke. I’ve been on atorvastatin for 8 years. My lipase is always normal. This is just fearmongering. You people don’t understand pharmacology. If it was that dangerous, it wouldn’t be approved. The FDA doesn’t approve death traps.
Danielle Stewart
December 26, 2025 AT 00:08For anyone on multiple meds-especially if you’re over 60 or have chronic illness-keep a printed list. Carry it in your wallet. Show it to every new doctor. Don’t assume they’ll check your chart. Most clinics still use paper records. You are your own best advocate. I’ve saved three friends just by asking, ‘Did you check for drug interactions?’
Ryan van Leent
December 27, 2025 AT 10:10So let me get this straight if I take lisinopril and get pancreatitis its my fault for not knowing every possible side effect of every pill I take? Why dont they just put a skull and crossbones on the bottle? Why do we have to be medical detectives just to stay alive
jessica .
December 28, 2025 AT 06:35Big Pharma knows this. They’ve known for decades. The FDA is a puppet. They don’t care if you die as long as the stock price goes up. Look at the opioid crisis. Same playbook. They’ll bury the data, pay off the doctors, and keep selling. You think this is an accident? It’s a business model.
Chris Davidson
December 29, 2025 AT 05:09People need to stop blaming drugs. The real issue is poor lifestyle. Obesity. Sedentary habits. Poor diet. That’s what causes pancreatitis. Medications are just convenient scapegoats. If you want to stay healthy, stop taking pills and start eating vegetables.
shivam seo
December 30, 2025 AT 01:47Why are Americans so obsessed with pills? In Australia we don’t pop meds like candy. We fix the root cause. Eat real food. Move your body. Sleep. But no, you’d rather swallow a chemical and call it healthcare. This is why your life expectancy is dropping. You’re medicating symptoms instead of living.
Andrew Kelly
December 30, 2025 AT 11:17Everyone’s panicking about meds but no one’s talking about the real culprit: the gut microbiome. Modern antibiotics, processed food, and stress wreck your microbiome. That’s what causes inflammation. The drugs are just the final trigger. If your gut’s healthy, your pancreas won’t react. It’s not the drug-it’s your body being broken by modern life.
Frank Drewery
December 31, 2025 AT 12:00I had this happen. Took exenatide for diabetes. Three weeks in, started getting dull pain after meals. Went to my doctor. He said ‘it’s probably gas.’ I pushed for a lipase test. It was 1,800. Stopped the drug. Two weeks later, back to normal. No damage. But if I’d listened to him, I’d be dead. Don’t wait. Ask for the test. It’s a simple blood draw. It could save your life.