
Choosing a mood‑stabiliser for bipolar disorder feels a bit like picking a travel companion - you need someone reliable, low‑maintenance and safe for the long haul. Lamictal Dispersible vs alternatives is the question many patients and carers ask when the doctor first mentions lamotrigine. This guide breaks down how Lamictal Dispersible (lamotrigine) stacks up against the most widely used alternatives, so you can see where each one shines and where it might fall short.
Lamictal Dispersible is the oral‑dispersible tablet form of lamotrigine, an anticonvulsant approved for both epilepsy and the maintenance treatment of bipolar disorder. Its key advantage is a low risk of causing weight gain, and it has the reputation of being gentle on cognition. First approved in the U.S. in 1994, the dispersible tablet was introduced in the UK in 2018 to help patients who struggle with swallowing pills.
Quick Takeaways
- Lamictal Dispersible works by stabilising neuronal firing without the heavy sedation of many antipsychotics.
- It climbs slowly - titration can take up to 8‑12 weeks - which reduces the risk of a potentially serious rash.
- Alternatives like lithium, valproate, carbamazepine, quetiapine and oxcarbazepine each have unique strengths (e.g., rapid mood‑episode control) and trade‑offs (e.g., weight gain, organ monitoring).
- Pregnancy safety varies: lamotrigine is considered relatively safe, while valproate is generally avoided.
- Side‑effect profiles and drug‑interaction potentials should guide the final choice, alongside personal health history.
How Lamotrigine Works
Lamotrigine inhibits voltage‑gated sodium channels, which dampens the excessive release of excitatory neurotransmitters like glutamate. This mechanism helps smooth out the rapid swings that characterize bipolar disorder, especially the depressive phases that many other stabilisers struggle with.
Common Alternatives at a Glance
Before diving into the side‑by‑side table, here’s a brief snapshot of each contender.
- Lithium - the classic mood stabiliser, renowned for its anti‑suicidal properties but demanding regular blood‑level checks.
- Valproate (Divalproex Sodium) - a broad‑spectrum anticonvulsant that calms manic spikes quickly, yet carries risks for liver toxicity and birth defects.
- Carbamazepine - effective for mixed‑episode patients, but notorious for drug interactions and a possible rash.
- Quetiapine - an atypical antipsychotic that also works as a mood stabiliser, often chosen for its sedative effect.
- Oxcarbazepine - a newer cousin of carbamazepine with a slightly cleaner side‑effect profile, used off‑label for bipolar maintenance.
| Medication | Primary Mechanism | FDA/EMA Indication for Bipolar | Typical Maintenance Dose | Key Side Effects | Pregnancy Safety |
|---|---|---|---|---|---|
| Lamictal Dispersible | Na⁺ channel inhibition | Yes (maintenance) | 100‑200mg daily (after titration) | Rash (rare SJS), dizziness, headache | Category C - generally acceptable |
| Lithium | Modulates second‑messenger systems | Yes (maintenance) | 600‑1200mg daily (serum 0.6‑1.0mEq/L) | Thyroid, renal, tremor, weight gain | Category D - use only if benefits outweigh risks |
| Valproate | Increases GABA, blocks Na⁺ channels | Yes (mania) | 500‑1500mg daily | Liver toxicity, weight gain, hair loss | Category X - contraindicated in pregnancy |
| Carbamazepine | Na⁺ channel blockade | Yes (maintenance, off‑label) | 200‑600mg daily | Rash, hyponatremia, enzyme induction | Category D - cautious use |
| Quetiapine | D2 & 5‑HT2A antagonism | Yes (depression & mania) | 300‑600mg daily | Sedation, metabolic changes, EPS | Category C - relatively safe |
| Oxcarbazepine | Na⁺ channel blockade (similar to carbamazepine) | Off‑label for bipolar | 300‑1200mg daily | Hyponatremia, dizziness | Category C - moderate safety |
In‑Depth Look at Each Option
Lamictal Dispersible (Lamotrigine)
Pros:
- Excellent for preventing depressive relapses - data from a 2022 meta‑analysis show a 35% reduction in depressive episode recurrence.
- Minimal weight gain; some patients even lose a few pounds.
- Low cognitive fog compared with many antipsychotics.
Cons:
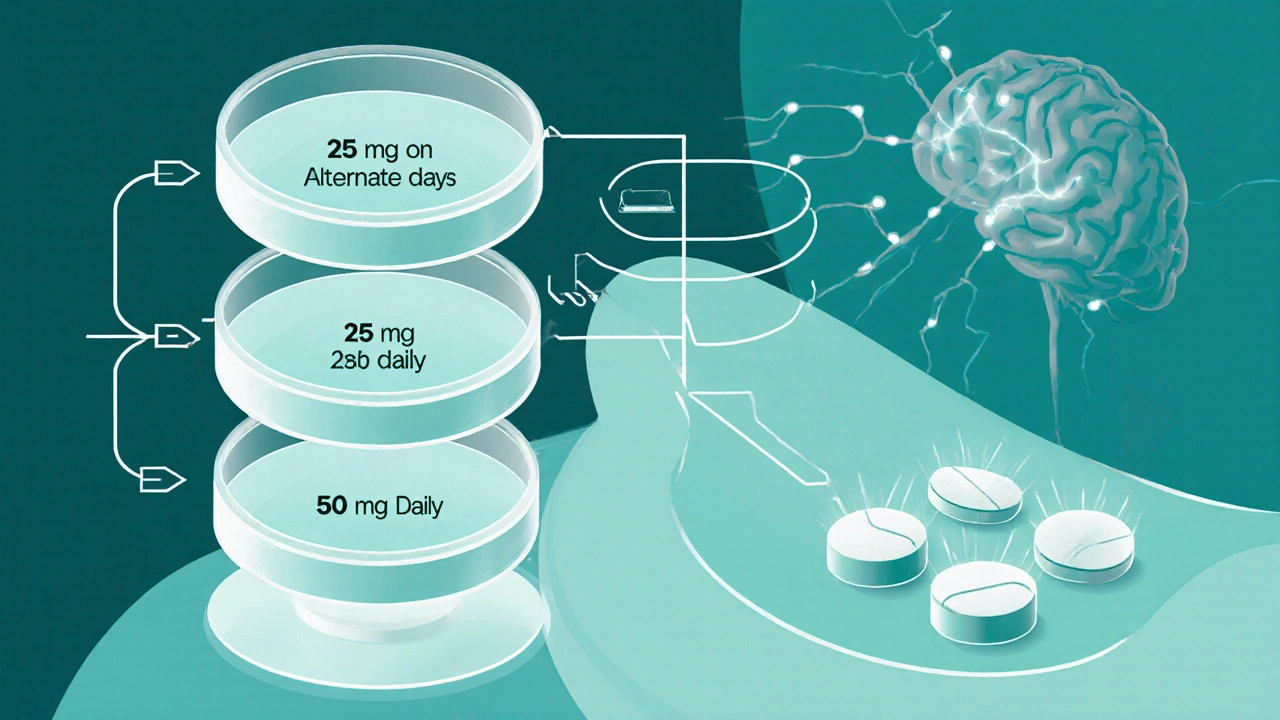
- Slow titration required to avoid Stevens‑Johnson‑like rashes - typical schedule: 25mg every other day for two weeks, then 25mg daily for two weeks, then 50mg daily.
- Skin reactions, though rare, can be severe.
- Not as effective for acute mania; usually paired with a rapid‑acting agent.
Lithium
Pros:
- Strong evidence for reducing suicide risk - a 2020 systematic review found a 48% drop in suicidal behavior.
- Good at stabilising both mania and depression when serum levels are optimal.
Cons:
- Narrow therapeutic window - requires regular blood draws.
- Potential kidney and thyroid problems over long‑term use.
- Weight gain and tremor are common complaints.
Valproate (Divalproex Sodium)
Pros:
- Rapid control of manic symptoms - useful in acute episodes.
- Fewer monitoring visits than lithium.
Cons:
- Teratogenic - linked to neural‑tube defects, thus avoided in women of child‑bearing age.
- Weight gain, hair thinning, and liver enzyme elevation are frequent.
Carbamazepine
Pros:
- Effective for mixed‑state and rapid‑cycling patients.
- Can also treat comorbid seizures.
Cons:
- Enzyme inducer - reduces levels of many other drugs, including oral contraceptives.
- Risk of serious rash (including Stevens‑Johnson) similar to lamotrigine.
- Hyponatremia in older adults.
Quetiapine
Pros:
- Provides both mood‑stabilising and sedative effects - helpful for insomnia.
- Approved for bipolar depression, so it covers both poles.
Cons:
- Weight gain, elevated glucose, and lipid changes are common.
- May cause daytime drowsiness.
Oxcarbazepine
Pros:
- Similar efficacy to carbamazepine with fewer drug‑interaction problems.
- Better tolerated in patients with liver concerns.
Cons:
- Hyponatremia risk, especially in the elderly.
- Limited bipolar‑specific data; often used off‑label.
Decision‑Making Framework
When you or your clinician weigh options, consider these five buckets.
- Efficacy for the targeted mood phase. Lamotrigine shines for depression; lithium and valproate are stronger for mania.
- Side‑effect tolerance. If weight gain is a deal‑breaker, avoid valproate and quetiapine.
- Monitoring burden. Lithium and carbamazepine demand blood work; lamotrigine’s main monitoring is rash vigilance.
- Pregnancy considerations. Lamotrigine and lithium (Category D) are more acceptable than valproate (Category X).
- Drug‑interaction profile. Carbamazepine and oxcarbazepine induce enzymes; they can lower the effectiveness of oral contraceptives or other psychotropics.
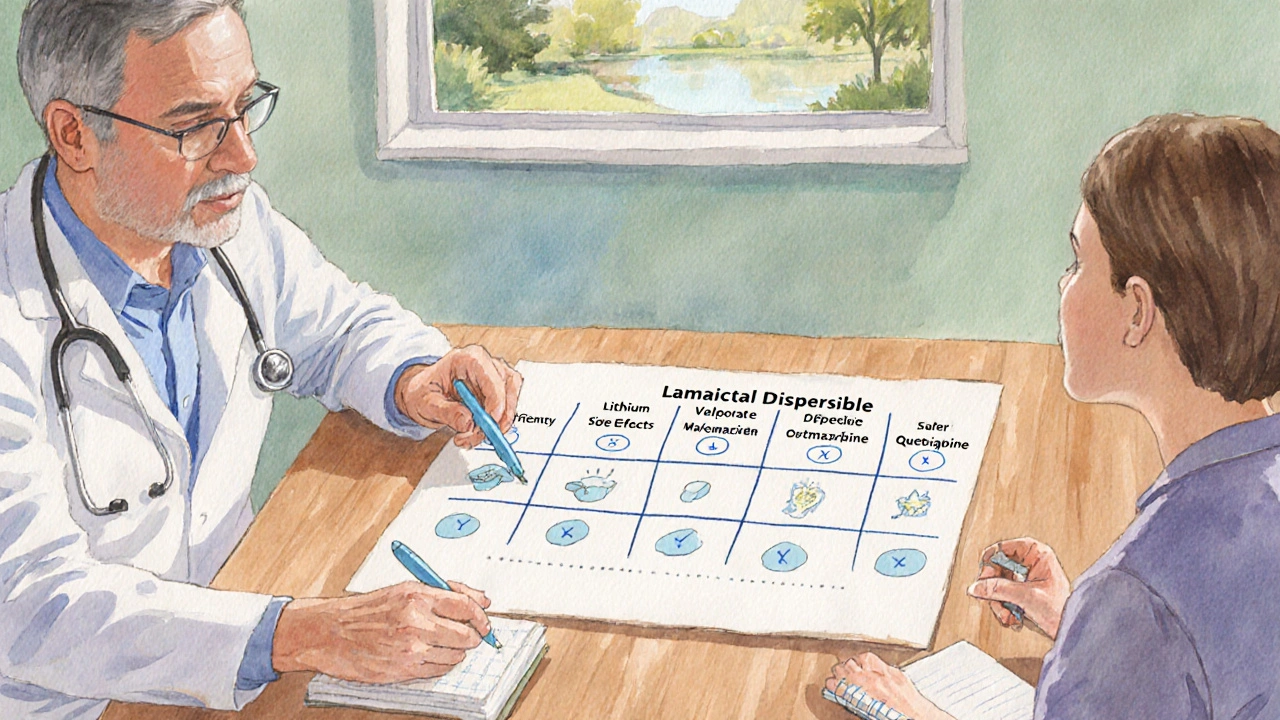
Plotting these factors on a simple matrix (high‑impact vs low‑impact) often makes the right choice clearer.
Practical Tips for Switching or Adding Lamotrigine
Many patients start with a different mood stabiliser and later add lamotrigine for depressive coverage. Below is a step‑by‑step plan that aligns with UK NICE guidelines.
- Confirm current medication’s serum level (e.g., lithium) is stable.
- Start lamotrigine 25mg on alternate days for two weeks.
- Increase to 25mg daily for another two weeks.
- Raise to 50mg daily for two weeks, then to the target 100‑200mg based on response and tolerability.
- Monitor skin weekly; advise the patient to report any rash immediately.
- If a rash appears, stop lamotrigine and seek urgent medical advice - re‑challenge is only possible after full resolution and a supervised plan.
Always coordinate with the prescribing psychiatrist or GP to avoid overlapping toxic levels.
Next Steps & Troubleshooting
If you’ve read this far, you probably have a medication in mind and a few lingering questions. Here’s what to do next:
- Schedule a medication review. Bring this comparison sheet to your appointment - it helps the clinician see where you stand.
- Request baseline labs. For lithium, check kidney function and thyroid; for valproate, get liver enzymes.
- Track side effects. Use a simple diary: date, dose, symptom severity (1‑10). Patterns emerge quickly.
- Consider lifestyle factors. Smoking can affect carbamazepine levels; alcohol can worsen lithium toxicity.
- Plan for pregnancy. If child‑bearing is a possibility, discuss switching to lamotrigine well before conception.
Frequently Asked Questions
Can I take lamotrigine and lithium together?
Yes, many clinicians combine them to cover both poles of bipolar disorder. Lamotrigine handles depression while lithium stabilises mania and reduces suicide risk. Regular blood draws for lithium are still required, but no major pharmacokinetic interaction is known.
Why does lamotrigine need such a slow titration?
The slow increase lowers the chance of a severe skin reaction called Stevens‑Johnson syndrome. Studies show the risk drops from ~0.1% with rapid titration to <0.01% when the standard 8‑week schedule is followed.
Is quetiapine a good first‑line choice for bipolar depression?
Quetiapine is approved for bipolar depression and works fast, but the side‑effect load (weight, metabolic changes) makes many clinicians prefer lamotrigine as a first‑line option, reserving quetiapine for patients who also need sleep aid.
What monitoring is needed for carbamazepine?
Baseline CBC, liver function, and sodium level are recommended. Then check sodium and liver enzymes every 3‑6months, especially in the first year.
If I’m pregnant, which mood stabiliser is safest?
Lamotrigine (Category C) and lithium (Category D) are the most frequently used during pregnancy, but both require careful monitoring. Valproate is contraindicated due to high birth‑defect risk.

Darin Borisov
October 14, 2025 AT 02:00One must appreciate the ontological stratification of mood‑stabilising pharmacotherapy, wherein lamotrigine occupies a niche of neurophysiological modulation that is both synaptic and network‑centric; this is not merely a matter of titration schedules but an intricate choreography of voltage‑gated sodium channel dynamics that reverberates through excitatory pathways. The literary comparison to a travel companion, while whimsical, belies the profound pharmacokinetic elasticity inherent in the dispersible formulation, facilitating adherence in populations historically disenfranchised by dysphagia. Moreover, the negligible propensity for weight gain situates lamotrigine as a paragon of metabolic neutrality, a characteristic that in the lexicon of psychiatric treatment is tantamount to a fiscal surplus in quality‑adjusted life years. Its cognitive sparing effects further demarcate a departure from the anticholinergic burden typical of many atypical antipsychotics, thereby preserving executive function for the quotidian exigencies of occupational performance. Indeed, the protracted titration curve-spanning eight to twelve weeks-serves as a prophylactic algorithm against the immunopathology of Stevens‑Johnson syndrome, a risk calculus that must be weighted against the therapeutic yield in depressive relapse mitigation. The empirical meta‑analysis cited, indicating a 35% decrement in depressive episode recurrence, is not an anecdotal artefact but a statistically robust datum derived from heterogeneous cohorts across multiple continents. In juxtaposition, lithium’s anti‑suicidal efficacy, while laudable, is encumbered by its nephrotoxic and thyroidal sequelae, compelling clinicians to negotiate a precarious therapeutic window. Valproate, albeit efficacious in acute mania, invokes teratogenic considerations that render it unsuitable for women of child‑bearing potential, a demographic consideration often marginalized in clinical trial design. Carbamazepine’s enzymatic induction profile, with its propensity to attenuate concomitant psychotropic plasma concentrations, introduces a layer of polypharmacy complexity that can destabilise the delicate equilibrium of mood regulation. Quetiapine’s sedative proclivity, while therapeutically advantageous for insomnia comorbidity, risks metabolic derangements that are antithetical to cardiovascular health. Oxcarbazepine, though a structural analogue with an ostensibly cleaner side‑effect spectrum, suffers from a paucity of bipolar‑specific evidence, relegating its use to off‑label conjecture.
Consequently, the decision‑making matrix espoused in the guide provides a heuristic scaffold upon which clinicians can overlay patient‑centric variables-efficacy, side‑effect tolerance, monitoring burden, teratogenic risk, and drug‑interaction profiles-to converge upon an optimal pharmacological regimen. The strategic incorporation of lamotrigine as a depressive prophylactic, synergistically paired with lithium for manic prophylaxis, epitomises a rational polypharmacy paradigm that maximizes therapeutic breadth while minimising adverse impact. Ultimately, the confluence of empirical evidence, mechanistic insight, and individualized patient narratives coalesce to inform a nuanced, evidence‑based selection of mood stabilisers.
Sean Kemmis
October 14, 2025 AT 15:53Honestly this guide is too much fluff for what should be a simple choice.
Nathan Squire
October 15, 2025 AT 05:46While the prose may appear labyrinthine, the underlying pharmacodynamics are elegantly straightforward: lamotrigine mitigates excitatory glutamatergic overflow without the sedative collateral of many antipsychotics. One must, however, commend the author for addressing the titration conundrum, an aspect often omitted in patient‑facing literature. The comparative tables, though dense, serve as an empirical Rosetta Stone for clinicians navigating the polypharmacy maze. It is also noteworthy that the guide refrains from promulgating a one‑size‑fits‑all mantra, instead advocating a personalized algorithmic approach. In essence, the treatise balances academic rigor with pragmatic guidance, a rare feat in patient education.
satish kumar
October 16, 2025 AT 09:33Really? All this detail seems overkill when most patients just want to know which pill won’t make them gain weight.
Adam Craddock
October 16, 2025 AT 23:26The emphasis on weight neutrality is indeed a salient point, especially given the psychosocial impact of obesity on mental health.
SHIVA DALAI
October 17, 2025 AT 13:20I feel like this guide finally gives my anxiety the closure it needed.
Vikas Kale
October 18, 2025 AT 03:13From a pharmacokinetic perspective, the slow titration of lamotrigine is a classic case of dose‑response optimisation 🧪. The renal clearance profile is modest, reducing the need for aggressive monitoring relative to lithium’s serum level surveillance. Moreover, the drug‑interaction matrix shows minimal CYP450 involvement, which mitigates contraindications with oral contraceptives – a crucial consideration for many patients. In practice, these attributes translate to a streamlined therapeutic regimen with a favorable safety margin.
Deepak Bhatia
October 18, 2025 AT 17:06Great overview! It’s reassuring to see the emphasis on gentle side‑effects and practical tips for switching.
Luke Dillon
October 19, 2025 AT 07:00Thanks for the clear step‑by‑step plan – it makes the titration process feel much less intimidating.
Elle Batchelor Peapell
October 19, 2025 AT 20:53Interesting how the guide balances scientific nuance with plain‑language explanations – a rare combo in med‑talk.
Jeremy Wessel
October 20, 2025 AT 10:46Short and sweet: lamotrigine for depression, lithium for mania, monitor accordingly.
Dustin Richards
October 21, 2025 AT 00:40The systematic framing of decision‑making criteria is commendable; it provides a structured approach for clinicians to align therapeutic choices with individual patient profiles.
Vivian Yeong
October 21, 2025 AT 14:33While thorough, the guide could benefit from a more concise summary for quick reference.