
When you start taking opioids for chronic pain, you’re told about the risks: drowsiness, nausea, addiction. But one of the most common and frustrating side effects? Constipation. And it doesn’t go away. Unlike nausea, which fades after a few days, opioid-induced constipation sticks around for as long as you’re on the medication. Up to 95% of people on long-term opioids deal with it. And most doctors don’t talk about it until it’s already a problem.
Why Opioids Cause Constipation (And Why Regular Laxatives Often Fail)
Opioids bind to receptors in your gut, not just your brain. These receptors control how your intestines move, how much fluid gets absorbed, and how quickly food passes through. When they’re activated, your bowels slow down. Secretions drop. Water gets sucked out of stool. The result? Hard, dry, painful bowel movements that feel impossible to pass. Here’s the catch: regular constipation treatments often don’t work well for this. Increasing fiber? Sounds logical, right? But in OIC, fiber can make things worse. Opioids already slow gut movement, so fiber ferments in the intestines, causing bloating, gas, and even fecal impaction. Studies show 25-40% of patients get more symptoms when they try high-fiber diets. Even over-the-counter laxatives like senna or Miralax only help about half the time. Why? Because they don’t target the root cause. They just try to force things along. But if the gut’s muscles are frozen by opioids, pushing harder doesn’t help-it just causes cramping.What Actually Works: The Step-by-Step Approach
Doctors now recommend a clear, step-based plan. It starts before you even take your first opioid pill. Step 1: Assess Before You Start Before beginning opioid therapy, your provider should check your baseline bowel habits. Tools like the Bristol Stool Form Scale (which rates stool from type 1-hard lumps-to type 7-watery) help track changes. If you’re already constipated, you need treatment before opioids are even prescribed. Step 2: Start With the Right Laxatives First-line treatment isn’t random. The best evidence points to:- Polyethylene glycol (PEG) - 17-34 grams daily. This is the gold standard. It draws water into the colon without irritating the gut.
- Bisacodyl or senna - Stimulant laxatives. Use these if PEG alone isn’t enough. Don’t use them long-term unless needed.
| Drug (Brand) | Form | Approved For | Onset of Action | Common Side Effects | Monthly Cost (USD) |
|---|---|---|---|---|---|
| Methylnaltrexone (Relistor®) | Injection | Palliative care, advanced illness | 30 minutes to 4 hours | Injection site pain, dizziness | $800-$1,200 |
| Naloxegol (Movantik®) | Oral tablet | Chronic non-cancer pain | 25 minutes to 24 hours | Abdominal pain, diarrhea | $700-$1,000 |
| Naldemedine (Symcorza®) | Oral tablet | Chronic non-cancer pain | Within 24 hours | Abdominal pain, diarrhea | $500-$800 |
| Lubiprostone (Amitiza®) | Oral capsule | Women, then men (off-label) | 24-48 hours | Nausea (30%), diarrhea (15-20%) | $600-$900 |
What Patients Are Really Saying
On patient forums, the frustration is real. Reddit users in r/ChronicPain say they’ve tried everything: Miralax, senna, prune juice, magnesium, even enemas. Most say none of it lasts. One user wrote: “I take 100mg of oxycodone a day. I’ve been on Miralax for two years. I still go maybe once every 5 days. I feel like I’m carrying bricks inside me.” Methylnaltrexone gets praised for speed-some say relief in under an hour. But the injection is a barrier. People hate needles. And at $1,000 a month, insurance often denies it unless you’ve tried everything else. Naldemedine (Symcorza®) has better ratings. Patients report more consistent relief and no shots. But 38% still get abdominal pain. That’s a trade-off: better bowel movements, but stomach discomfort. The big complaint? Trial and error. No one tells you which drug to try first. You end up spending months testing options, paying out of pocket, and feeling like your body is broken.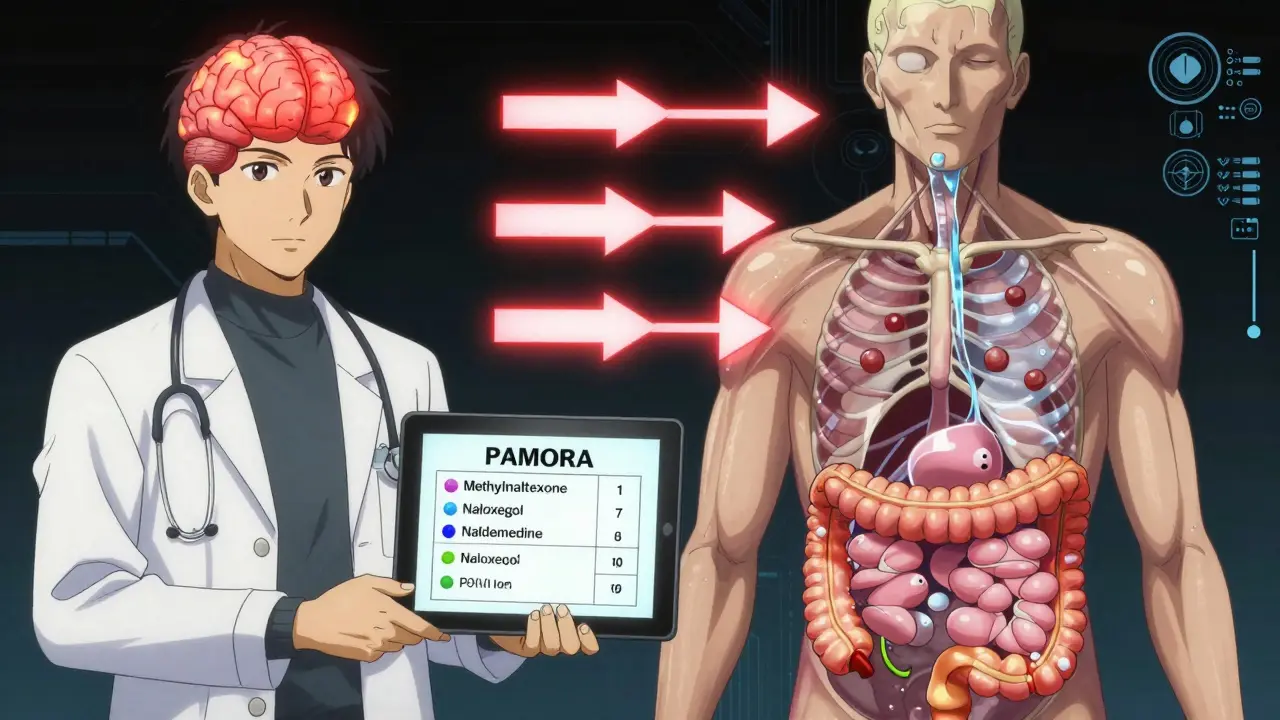
Why So Many People Go Untreated
Even though guidelines exist, most doctors don’t follow them. A 2023 AMA survey found only 22-35% of community practices use standardized OIC assessment tools. Nurses, who see patients daily, say 80% of them would use simpler protocols-but only 19% of doctors agree. Why? Time. Training. Lack of reimbursement. Many providers think, “It’s just constipation. Give them a laxative.” But that’s like treating a broken leg with a bandage. Also, opioids come with FDA-mandated Risk Evaluation and Mitigation Strategies (REMS). Since 2022, these include OIC education. But many prescribers still skip it. The result? Thirty to forty percent of patients reduce or stop their opioids-not because the pain isn’t controlled, but because constipation is unbearable. That’s a huge loss. Pain management fails when bowel function fails.What You Can Do Right Now
If you’re on opioids and struggling with constipation:- Start with polyethylene glycol (Miralax) at 17g daily. Increase to 34g if needed.
- Drink at least 2 liters of water a day. Laxatives need water to work.
- Don’t add fiber unless your doctor says so. It might make things worse.
- Track your bowel movements daily. Use the Bristol Scale. Take a photo if needed.
- If no improvement after 7 days, ask your doctor about PAMORAs.
- Ask if your insurance covers naldemedine or naloxegol. They’re often cheaper than methylnaltrexone.
The Future Is Coming
New treatments are on the horizon. A fixed-dose combo of naloxone and polyethylene glycol is in Phase III trials. If approved in 2024, it could be the first pill that both relieves constipation and reduces opioid tolerance. Also, naldemedine was approved for kids in March 2023. That opens the door for pediatric pain patients-something no one talked about five years ago. The market for OIC drugs is expected to hit $3.4 billion by 2028. More options are coming. But until then, you need to be your own advocate.Frequently Asked Questions
Is opioid-induced constipation the same as regular constipation?
No. Regular constipation is often caused by low fiber, dehydration, or inactivity. Opioid-induced constipation (OIC) is caused by opioids directly slowing gut movement and reducing fluid secretions. Standard treatments like fiber or stimulant laxatives often fail because they don’t address the root mechanism. OIC requires targeted therapies like PAMORAs or osmotic laxatives like polyethylene glycol.
Can I just use Miralax long-term for OIC?
Yes, polyethylene glycol (Miralax) is safe for long-term use in OIC. Unlike stimulant laxatives (e.g., senna), it doesn’t irritate the gut or cause dependency. It’s actually the first-line recommendation. But if you’re still having trouble after 7-10 days at the full dose (34g/day), you likely need a stronger option like a PAMORA. Don’t wait months to ask for help.
Why won’t my insurance cover methylnaltrexone or naldemedine?
Most insurers require step therapy: you must try and fail at least two over-the-counter laxatives and possibly one prescription laxative before approving a PAMORA. Some also require proof that you’ve tried increasing fluid and activity. Your doctor can submit a prior authorization letter citing clinical guidelines and your failed trials. Many patients get approved after one appeal.
Does taking laxatives reduce my opioid’s pain relief?
No, standard laxatives like Miralax or senna don’t interfere with opioid pain relief. They work in the gut, not the brain. PAMORAs like naldemedine and naloxegol are designed to block opioid receptors only in the intestines. They cross the blood-brain barrier too poorly to affect pain control. You can take them safely without losing pain management.
Should I stop my opioid if constipation gets too bad?
Don’t stop on your own. Up to 40% of patients reduce or quit opioids because of unmanaged constipation-even when their pain is under control. That’s dangerous. Instead, talk to your doctor about switching to a PAMORA or adjusting your laxative regimen. There are effective options. You don’t have to choose between pain relief and bowel function.
Next Steps
If you’re on opioids and constipated:- Start tracking your bowel movements today.
- Begin polyethylene glycol at 17g daily.
- Ask your doctor if you qualify for a PAMORA.
- Request a copy of the Bristol Stool Scale to use at home.
- Bring this information to your next appointment. You’re not being difficult-you’re being informed.

Josh josh
January 26, 2026 AT 08:43bro i took oxycodone for a year and just started taking miralax every day and it was like night and day
no more feeling like my intestines are made of concrete
why does no one tell you this upfront
Uche Okoro
January 26, 2026 AT 18:56The pathophysiology of opioid-induced constipation (OIC) is mediated by μ-opioid receptor (MOR) agonism in the enteric nervous system, resulting in reduced peristalsis, increased non-propulsive contractions, and diminished secretory activity-collectively termed 'gut hypomotility.' Standard osmotic laxatives like PEG exert their effect via colonic water retention, bypassing neuromuscular dysfunction. However, the clinical efficacy of PAMORAs such as naloxegol and naldemedine lies in their peripherally restricted antagonism of MORs in the GI tract, preserving central analgesia while restoring colonic transit time. The pharmacokinetic profile of naldemedine, with its high P-glycoprotein efflux and negligible CNS penetration, makes it particularly suitable for chronic non-cancer pain populations. The 2023 JAMA Internal Medicine meta-analysis confirmed a 47% increase in spontaneous bowel movements vs placebo with PAMORA use, with diarrhea as the most common AE (RR 2.1; 95% CI 1.7–2.6).