
When you take a sleep medication to finally get some rest, the last thing you expect is for your evening glass of wine to turn into a life-threatening mistake. But combining alcohol with prescription or over-the-counter sleep aids isn’t just a bad idea-it’s dangerously common, and the science behind it is terrifying.
Why This Combination Is So Risky
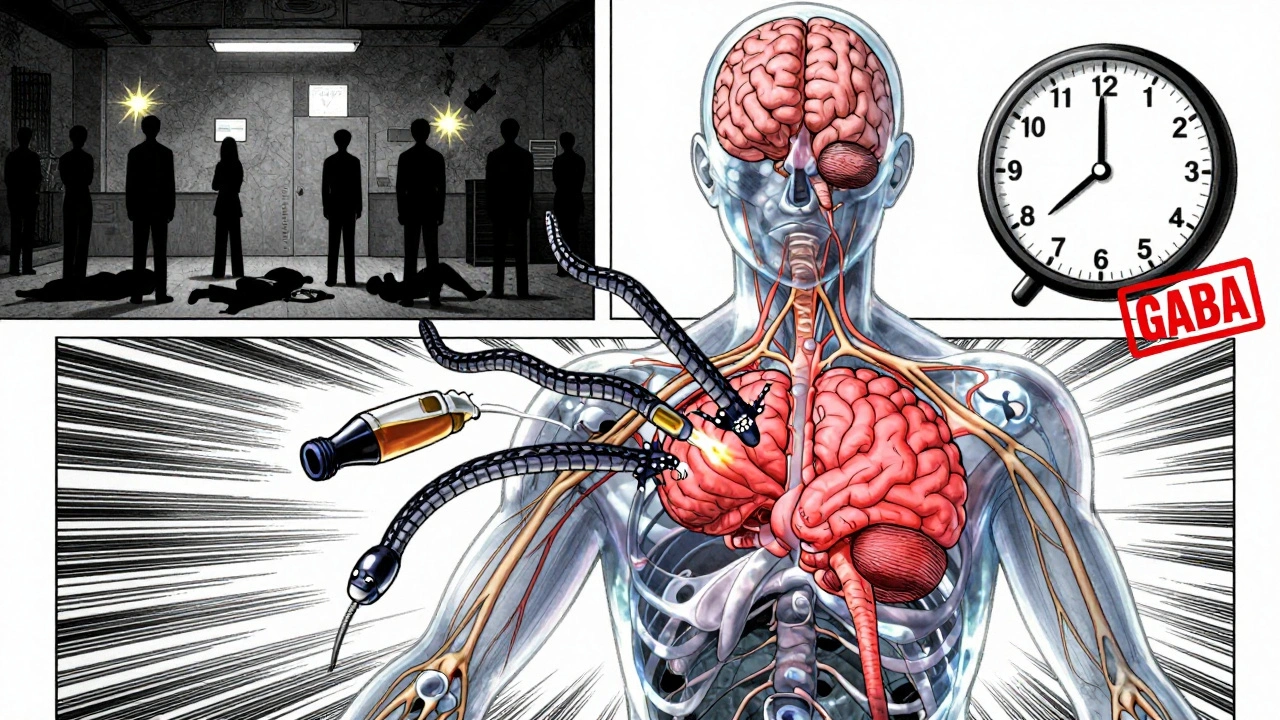
Alcohol and sleep medications don’t just add up-they multiply. Both are central nervous system depressants. They slow down your brain, your breathing, and your heart rate. When taken together, they don’t just make you drowsy. They can shut down your body’s most basic survival functions. The real danger comes from how they interact at the molecular level. Both alcohol and medications like Ambien (zolpidem), Lunesta (eszopiclone), and even common OTC sleep aids like diphenhydramine work by boosting the effect of GABA, a calming neurotransmitter in your brain. Alcohol doesn’t just add to this effect-it supercharges it. Studies show that even one drink can increase the sedative power of these drugs by up to 270%, far beyond what you’d expect from simply adding two substances together. This isn’t theoretical. In clinical trials, people who took zolpidem and consumed just one standard drink (14g of alcohol) saw their drug’s half-life jump from 2.5 hours to over 6 hours. That means the drug stays in your system much longer, keeping you groggy, confused, and at risk for hours after you thought it had worn off.Which Sleep Medications Are Most Dangerous With Alcohol?
Not all sleep meds are created equal when mixed with alcohol. The biggest risks come from three categories:- Z-drugs (zolpidem/Ambien, eszopiclone/Lunesta, zaleplon/Sonata): These are the most dangerous. The FDA issued a Black Box Warning for all of them, the strongest possible alert. Ambien-alcohol combinations alone made up 63% of emergency visits related to sleep med-alcohol interactions, even though they’re only 38% of prescriptions.
- Benzodiazepines (lorazepam/Ativan, clonazepam/Klonopin, temazepam/Restoril): These are older but still widely prescribed. They’re slightly less risky than Z-drugs, but still dangerous. One study showed they increase driving impairment by 1.9 times when mixed with alcohol.
- OTC sleep aids (diphenhydramine/ZzzQuil, doxylamine/Unisom): Many people think these are safe because they’re available without a prescription. They’re not. In adults over 65, mixing these with alcohol increases fall risk by 300%. Emergency room visits for hip fractures in this group jumped from 12.7 to 51.3 per 100,000 people when alcohol was involved.
Even melatonin, often seen as a “natural” alternative, isn’t risk-free. While it doesn’t cause dangerous respiratory depression like GABA-boosting drugs, it still increases next-day drowsiness by 35% when combined with alcohol-enough to make driving or operating machinery unsafe.
The Silent Killer: Respiratory Depression
The most frightening outcome isn’t just waking up groggy. It’s stopping breathing. A 2021 study in the Journal of Clinical Sleep Medicine tracked patients who took Lunesta with a blood alcohol level of 0.08%-the legal limit for driving. Their breathing dropped from a normal 16 breaths per minute to just 9.3. Oxygen levels fell to 84.7%, well below the safe threshold of 90%. That’s not just sleepy-that’s hypoxic. That’s the body slowly suffocating while asleep. In autopsy reports of fatal cases, the median blood alcohol level was 0.051%-less than half the legal driving limit. Many of these deaths happened because people thought “just one drink” was harmless. It wasn’t.Complex Sleep Behaviors: Waking Up Somewhere You Don’t Remember
Another terrifying side effect is performing complex tasks while asleep-called complex sleep behaviors. This includes sleep-driving, sleep-walking, cooking, or even having conversations without any memory of it afterward. The risk jumps from 0.15% with Z-drugs alone to 2.4% when alcohol is involved. That’s a 16-fold increase. Reddit threads are full of stories like one from a user named u/SleepWalker99: “I woke up 2 miles from home with no memory of driving there after taking half an Ambien with two glasses of wine.” The FDA has logged over 1,800 consumer complaints in a single year about this exact issue. Sixty-two percent of those who reported these incidents said they had “no memory of events.” That’s not just embarrassing-it’s legally and medically catastrophic.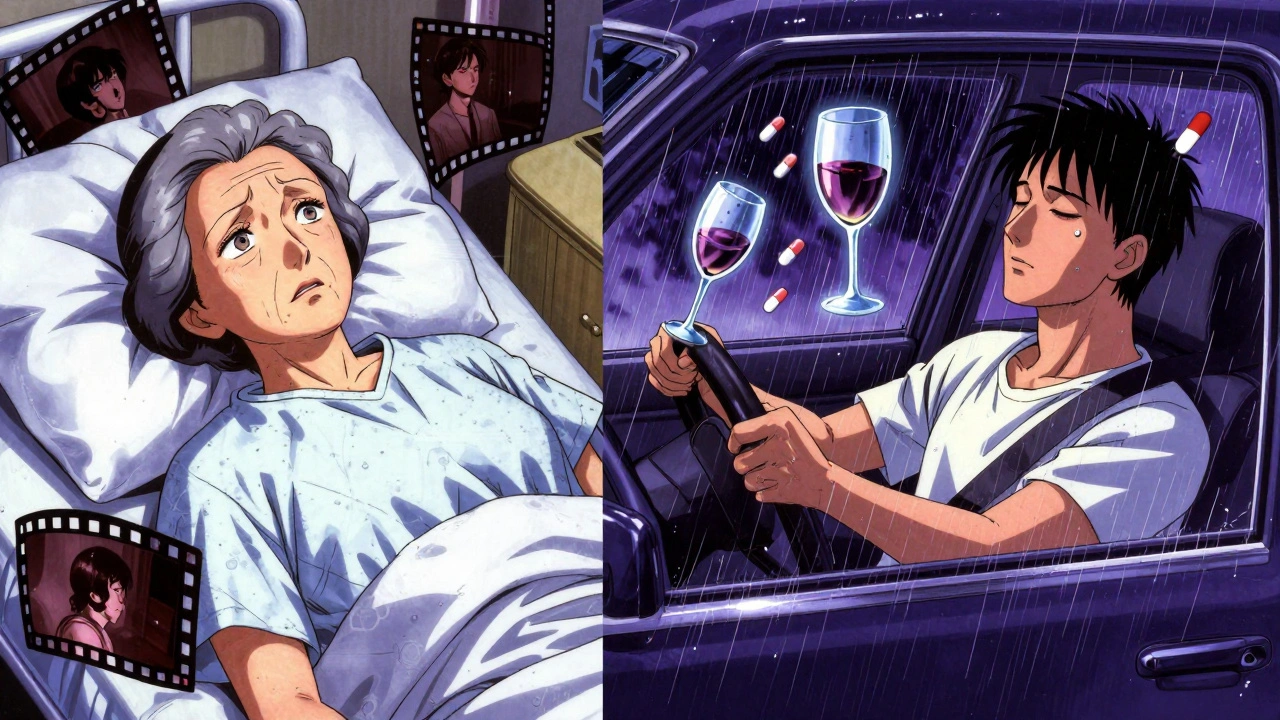
Why Older Adults Are at Highest Risk
Age changes how your body handles drugs and alcohol. As you get older, your liver processes both more slowly. Alcohol and sedatives stay in your system 40-60% longer. That means even small amounts become dangerous. The American Geriatrics Society updated its Beers Criteria in 2022 to say: Never use diphenhydramine or any sedating sleep aid with alcohol if you’re over 65. Why? Because the risk of delirium increases by 400%. One in three older adults who mix these substances ends up in the hospital with severe confusion, falls, or respiratory failure. AARP community forums are filled with heartbreaking stories: “I had one glass of wine with my Unisom and ended up in the ER, thinking I was in 1978.” “My dad forgot his own name after taking ZzzQuil with a beer.” These aren’t rare outliers-they’re predictable outcomes of a poorly understood interaction.What About Newer Sleep Meds?
There’s some hope. In 2023, the FDA approved Dayvigo (lemborexant), a new type of sleep medication that works differently. Instead of boosting GABA, it blocks orexin, a brain chemical that keeps you awake. In clinical trials, combining Dayvigo with alcohol only increased the drug’s half-life by 15%-compared to 150-200% for Z-drugs. It’s not a magic bullet, but it’s a step toward safer options. Seven out of the 12 sleep medications currently in clinical trials use non-GABA mechanisms, meaning they may avoid these deadly interactions entirely.What Should You Do?
The message from every major medical organization is clear: Don’t mix alcohol with any sleep medication. Not one drink. Not even a sip. If you’re prescribed a sleep aid:- Avoid alcohol completely while taking it.
- Wait at least 6 hours after taking a Z-drug before drinking alcohol. For benzodiazepines, wait 12 hours.
- If you’re over 65, avoid alcohol entirely if you’re on any sleep medication, even OTC ones.
- Ask your doctor or pharmacist: “Is this safe with alcohol?” Don’t assume they’ll tell you unless you ask.
A 2022 survey found that 68% of patients prescribed sleep meds received inadequate counseling about alcohol risks. That’s on the system. But you can protect yourself. Ask. Read the MedGuide. Look for the FDA’s Black Box Warning on the bottle.
What If You Already Mixed Them?
If you’ve taken alcohol and a sleep medication together:- Don’t drive. Don’t operate machinery.
- Don’t go to bed alone. Have someone stay with you.
- Watch for slow breathing, confusion, bluish lips, or unresponsiveness. If any of these happen, call 999 immediately.
- Even if you feel fine, the effects can build up hours later.
There’s no antidote. Treatment is supportive-oxygen, breathing support, monitoring. Prevention is the only real cure.
Alternatives That Are Actually Safe
If you’re using sleep meds because of alcohol-related insomnia, you’re caught in a cycle. Alcohol might help you fall asleep, but it destroys sleep quality. The next night, you’re more tired, so you take more medication-and the cycle worsens. Consider these safer, evidence-backed alternatives:- Cognitive Behavioral Therapy for Insomnia (CBT-I): The gold standard. More effective than pills long-term, with no side effects.
- Strict sleep schedule: Go to bed and wake up at the same time every day-even weekends.
- Reduce screen time before bed: Blue light suppresses melatonin.
- Limit caffeine after 2 PM: It lingers in your system for hours.
- Light exercise in the afternoon: Not right before bed, but enough to help regulate your rhythm.
These don’t promise instant results. But they fix the root problem-without risking your life.
Can I have one glass of wine with Ambien?
No. Even one standard drink with Ambien can dangerously increase sedation, slow your breathing, and cause you to perform complex tasks like driving without remembering it. The FDA’s Black Box Warning explicitly says this combination is contraindicated. There is no safe amount.
Is it safe to drink alcohol the next day after taking a sleep med?
It depends on the drug. For Z-drugs like Ambien or Lunesta, wait at least 6-8 hours. For benzodiazepines like Restoril, wait 12 hours or more. Older adults should wait longer-up to 24 hours-because metabolism slows with age. If you’re unsure, don’t take the risk.
Do OTC sleep aids like ZzzQuil interact with alcohol?
Yes, and the risk is especially high for people over 65. ZzzQuil contains diphenhydramine, which, when mixed with alcohol, increases fall risk by 300% and delirium risk by 400%. Many older adults end up in the ER after combining them, thinking it’s harmless.
What should I do if I accidentally mix alcohol and a sleep med?
Stay awake if possible. Don’t drive or go to bed alone. Have someone monitor you for slow breathing, confusion, or unresponsiveness. If breathing slows to fewer than 10 breaths per minute, lips turn blue, or you can’t wake up, call 999 immediately. There’s no antidote-only supportive care.
Are there any sleep aids that are safe with alcohol?
No prescription or OTC sleep aid that works by boosting GABA is safe with alcohol. Melatonin is the least risky, but it still increases next-day drowsiness by 35%. The safest option is to avoid alcohol entirely while using any sleep medication. Newer drugs like Dayvigo show promise with lower interaction risks, but they’re not risk-free.

michael booth
December 3, 2025 AT 15:14This is one of those topics that needs way more public awareness. I never realized how dangerous even one drink with Ambien could be. The 270% increase in sedation is insane. I'm sharing this with my family, especially my dad who's on sleep meds.
Carolyn Ford
December 4, 2025 AT 01:00Oh, please. You're scaremongering. I've had a glass of wine with my ZzzQuil for years. Nothing happened. People like you make everything sound like a horror movie. The real danger is fear-mongering that makes people avoid helpful meds altogether.
Heidi Thomas
December 5, 2025 AT 22:23Carolyn is right. This post is exaggerated. The FDA black box warning exists because of liability, not because it's actually dangerous. I work in pharmacy and see people panic over this every day. One drink doesn't kill you. It's the 10-drink binge that does. Stop treating normal behavior like a crime.
Alex Piddington
December 6, 2025 AT 11:07Thank you for this comprehensive breakdown. I appreciate how you laid out the science without sugarcoating it. Many people don't realize that 'natural' doesn't mean 'safe' - melatonin still interacts dangerously. I've shared this with my senior wellness group. We're updating our educational materials now.
Libby Rees
December 8, 2025 AT 05:40My grandmother took Unisom with a glass of wine every night. She fell last year and broke her hip. The ER doctor asked if she'd mixed it with alcohol. We didn't even know it was a risk. This post saved my family from future tragedy. Thank you.
Rudy Van den Boogaert
December 10, 2025 AT 05:10Just wanted to add something practical: if you're on any sleep med and you drink, don't just wait - track it. Use a pill tracker app. Set reminders. I use Medisafe. It tells me when it's safe to drink based on half-lives. It's not perfect, but it's better than guessing. Also, if you're over 60, skip the alcohol entirely. Your liver isn't what it was.
Martyn Stuart
December 12, 2025 AT 04:07Heidi, your comment is dangerously misleading. The 2021 JCSM study you're ignoring showed that at 0.08% BAC, breathing dropped to 9.3 breaths per minute - that's not 'scaremongering,' that's clinical hypoxia. And the FDA didn't issue a black box warning because of liability - they issued it because patients were dying. Please stop spreading misinformation.
Shofner Lehto
December 13, 2025 AT 12:48My doctor never told me about this interaction. I'm 52 and take Lunesta. I had a drink at dinner once - woke up at 3 a.m. with my head on the kitchen floor. No memory of how I got there. I haven't touched alcohol since. This isn't about fear - it's about respect for your body.
John Filby
December 14, 2025 AT 01:17Man, I thought I was being smart taking melatonin with wine. Turns out I'm just sleepy the next day? 😅 Thanks for the tip - I'm switching to CBT-I. No pills, no booze, just routine. My sleep's been better than ever. Also, no more Netflix in bed. Game changer.
Emmanuel Peter
December 15, 2025 AT 07:28So what? You're saying I can't have a beer after my Ambien? I'm not a child. I know my limits. You're treating adults like toddlers. The real problem is that people are too lazy to just sleep naturally - they want a pill and a drink and then cry when it backfires.
Ashley Elliott
December 15, 2025 AT 13:56Emmanuel, I get your frustration - but this isn't about control. It's about survival. I'm a nurse. I've seen three patients in the ICU this year from this exact combo. One was 78. He had one glass of wine. He didn't wake up. There's no pride in ignoring science. Please, just ask your doctor. It's not weakness - it's wisdom.