
When you need to prevent dangerous blood clots - whether from atrial fibrillation, deep vein thrombosis, or a mechanical heart valve - your doctor has two main choices: old-school Warfarin or one of the newer DOACs. Both work to stop clots, but they’re not the same. And when things go wrong - like a serious bleed - knowing how to reverse them can mean the difference between life and death.
How Warfarin Works (and Why It’s Still Around)
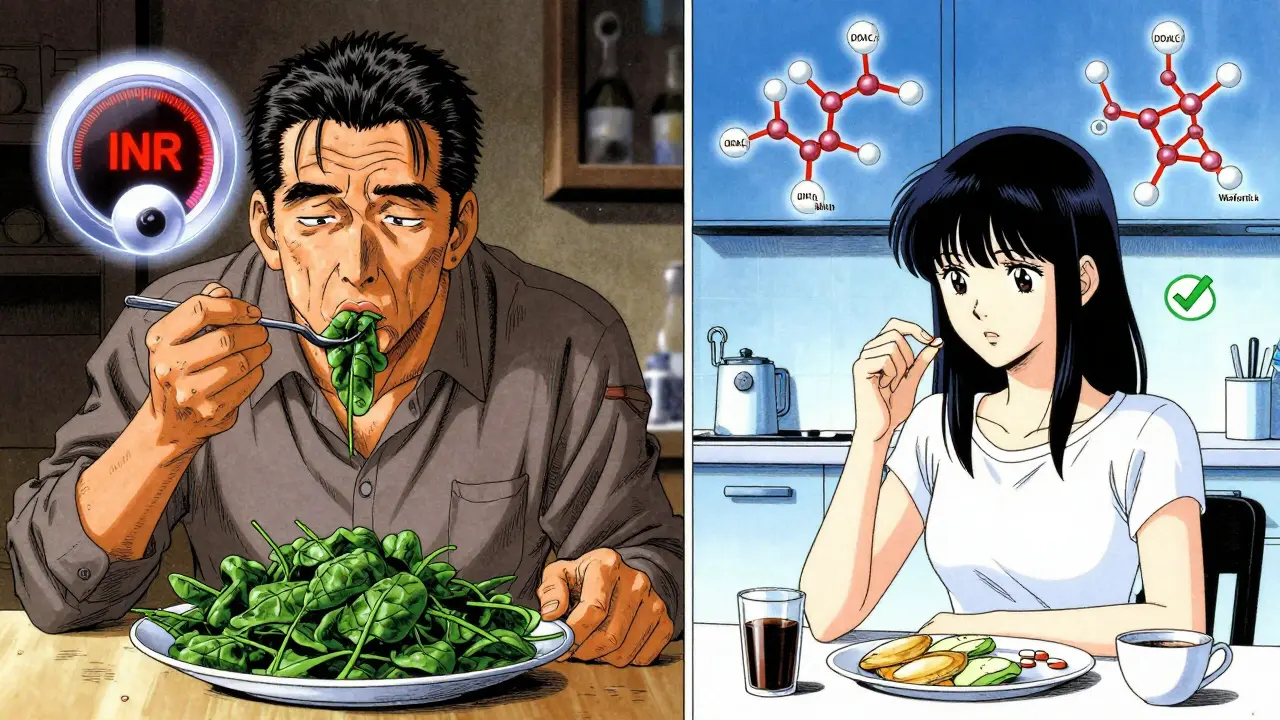
Warfarin has been around since the 1950s. It’s a vitamin K antagonist, meaning it blocks your body’s ability to use vitamin K to make clotting factors. That’s how it thins the blood. But here’s the catch: it’s a tightrope walk. Too little, and you’re at risk for a stroke or clot. Too much, and you could bleed internally - even from a minor bump.
To keep it safe, you need frequent blood tests. The standard is an INR between 2.0 and 3.0. For people with mechanical heart valves, that range jumps to 2.5-3.5. On average, someone on Warfarin gets their INR checked nearly 18 times a year. That’s not just inconvenient - it’s expensive and time-consuming.
And then there are the interactions. Warfarin clashes with hundreds of medications - from antibiotics to painkillers - and even foods. Spinach, kale, broccoli? High in vitamin K. One big salad can throw your INR off. That’s why people on Warfarin often feel like they’re on a diet they never signed up for.
What Are DOACs? And Why Are They Taking Over?
DOACs - direct oral anticoagulants - are the new kids on the block. Dabigatran, rivaroxaban, apixaban, edoxaban. These drugs skip the vitamin K pathway entirely. Instead, they target specific clotting factors: thrombin or factor Xa. That makes them more predictable.
They work faster. Most reach full effect in just 1-4 hours. No daily INR checks. No dietary restrictions. Fewer drug interactions. The University of Liverpool’s database shows Warfarin has over 300 major interactions. DOACs? Around 40. That’s a massive drop in complexity.
Since 2020, DOACs have been the first-line choice for most patients with non-valvular atrial fibrillation or venous thromboembolism. In the U.S., 85% of new anticoagulant prescriptions in 2023 were for DOACs. Why? Because the data says they’re better.
A 2023 JAMA study of nearly 18,500 people on long-term anticoagulation found DOACs reduced recurrent clots by 34% compared to Warfarin. Another meta-analysis of 35 studies showed DOACs cut major bleeding by 17%. Apixaban, in particular, slashed stroke risk by 25% and major bleeding by 35%.
When DOACs Fall Short
DOACs aren’t perfect. They’re not safe for everyone.
If you have a mechanical heart valve - especially a mitral valve - DOACs are off the table. Warfarin is still the only approved option. The same goes for people with antiphospholipid syndrome, where clots form even when INR is in range.
Severe kidney failure is another problem. Most DOACs are cleared by the kidneys. If your eGFR drops below 15 mL/min, they can build up to dangerous levels. Warfarin doesn’t care about kidney function - it’s metabolized by the liver. So in end-stage renal disease, Warfarin remains the go-to.
There’s also the cost. Warfarin costs $4 to $30 a month. DOACs? $300 to $500 without insurance. That’s why 34% of Medicare patients skip doses because they can’t afford them. The clinical benefits don’t matter if you can’t take the pill.
Reversal Agents: The Emergency Lifeline
When a patient on anticoagulants starts bleeding - say, from a fall, surgery, or a brain hemorrhage - you need to act fast. But reversing these drugs isn’t the same.
With Warfarin, you have options. Vitamin K (given IV) slowly rebuilds clotting factors. Fresh frozen plasma gives you all the clotting proteins at once. But the fastest and most reliable is prothrombin complex concentrate (PCC). It can normalize INR in under 30 minutes. That’s why ERs stock PCC.
DOACs are trickier. You can’t just give vitamin K - it won’t work. Each DOAC needs its own antidote.
Dabigatran? Idarucizumab (Praxbind®). It’s a monoclonal antibody that grabs dabigatran like a magnet. The RE-VERSE AD trial showed it reversed anticoagulation in 98.7% of patients with major bleeding. But it costs $3,400 per vial. And only 62% of U.S. hospitals keep it in stock.
Rivaroxaban, apixaban, edoxaban? These are factor Xa inhibitors. Andexanet alfa (Andexxa®) reverses them. It’s a modified version of factor Xa that soaks up the drug. But it’s even pricier - $17,000 per treatment. And again, availability is spotty, especially in rural areas.
If you don’t have the specific antidote? Use 4-factor PCC. It’s not as effective, but it’s better than nothing. Some hospitals use it as a backup. Others don’t have it at all.
There’s hope on the horizon. Ciraparantag is an experimental universal reversal agent that could work on all DOACs - and even heparin. It’s in Phase III trials and could be available by 2025. That would be a game-changer.
Who Should Take What?
Here’s the real-world breakdown:
- Choose DOACs if: You have non-valvular AF or VTE, normal kidney function, can afford the cost, and don’t want daily blood tests or dietary restrictions.
- Stick with Warfarin if: You have a mechanical heart valve, severe kidney failure (eGFR <15), antiphospholipid syndrome, or can’t afford DOACs but have reliable access to INR monitoring.
- Consider lower-dose DOACs if: You’re over 80, weigh less than 60kg, or have elevated creatinine. Apixaban 2.5mg twice daily is FDA-approved for this group and reduces bleeding risk without losing protection.
For frail elderly patients, DOACs cut intracranial bleeding by 45% compared to Warfarin. That’s huge. A brain bleed in an 85-year-old is often fatal. DOACs make that risk much lower.

What’s Next? The Future of Blood Thinners
The field is moving fast. New drugs are coming. Milvexian, a factor XIa inhibitor, showed 46% less bleeding than apixaban in a 2023 trial. It might be the next generation - effective, but safer.
DOACs are also being approved for cancer-related clots. The 2023 ASCO guidelines now recommend apixaban or rivaroxaban over low-molecular-weight heparin for most cancer patients. Why? Because they’re easier to take, and studies show they work just as well - with fewer complications.
Even in severe kidney disease, new data is changing old rules. The 2024 AUGUSTUS-CKD subanalysis found apixaban reduced major bleeding by 31% in dialysis patients - something we were told was too risky just a year ago.
By 2028, DOACs are expected to make up 82% of the anticoagulant market. Warfarin will be reserved for the few cases where it’s truly needed.
What You Should Do
If you’re on anticoagulants, ask yourself these questions:
- Do I know exactly which drug I’m taking - and why?
- Do I understand the signs of bleeding - black stools, headaches, unexplained bruising?
- Does my doctor know my kidney function and weight? Are they adjusting my dose?
- If I go to the ER, will they know how to reverse my medication?
Don’t assume your doctor automatically switched you to a DOAC. Ask. And if you’re on Warfarin, make sure your INR is checked regularly. Missing a test is dangerous.
Cost is a real barrier. Talk to your pharmacist. Ask about patient assistance programs. Some drugmakers offer free or discounted DOACs for low-income patients. Don’t skip doses just because you’re worried about the bill.
Anticoagulation isn’t just about taking a pill. It’s about knowing what to do when things go wrong. That’s why understanding your drug - and its reversal plan - isn’t optional. It’s life-saving.
Can I switch from Warfarin to a DOAC on my own?
No. Switching anticoagulants requires careful planning. Your doctor must overlap the drugs or use a bridge protocol to avoid gaps in protection or dangerous spikes in clotting risk. Never stop or switch without medical supervision.
Do DOACs require any monitoring at all?
Routine blood tests aren’t needed, but your doctor should check your kidney function at least once a year - and more often if you’re older or have other health issues. In emergencies, specialized blood tests (like anti-Xa assays) can measure DOAC levels, but they’re not part of regular care.
Is one DOAC better than the others?
Apixaban has the strongest safety data, especially for bleeding risk. Dabigatran has the most reliable reversal agent. Rivaroxaban and edoxaban are once-daily, which helps with adherence. The best choice depends on your kidney function, weight, other medications, and cost. Talk to your doctor about your priorities.
What should I do if I miss a dose of my DOAC?
If you miss a dose and it’s less than half the time until your next dose, take it right away. If it’s more than half the time, skip it and take your next dose at the regular time. Never double up. For apixaban or dabigatran (twice daily), missing one dose increases clot risk slightly - but doubling the next dose raises bleeding risk more. Consistency matters more than perfection.
Can I drink alcohol while on anticoagulants?
Moderate alcohol is usually okay - one drink a day for women, two for men. But heavy drinking raises bleeding risk, especially with Warfarin. Alcohol can also affect liver function, which changes how Warfarin is processed. If you drink regularly, tell your doctor. They may need to adjust your dose or switch you to a DOAC.

Prachi Chauhan
January 10, 2026 AT 21:50So basically we’re trading one set of problems for another? Warfarin’s a pain with the tests and food, but at least you know what you’re dealing with. DOACs? Fancy, fast, and expensive - but if something goes wrong, you’re stuck waiting for a drug that might not even be in your hospital.
Sona Chandra
January 11, 2026 AT 23:27THIS IS WHY AMERICA’S HEALTHCARE IS A JOKE. You get a life-saving drug that costs $500 a month and then act surprised when people skip doses? Who the hell thought this was a good idea? We’re literally letting people die because they can’t afford to live.
Cecelia Alta
January 12, 2026 AT 21:54Look, I get that DOACs are the new shiny thing, and sure, they’re easier - no INR checks, no kale anxiety - but let’s not pretend they’re magic. The reversal agents? Half the hospitals don’t have them. And if you’re in rural Nebraska or rural anywhere? Good luck. I’ve seen ER docs scrambling for Andexxa like it’s a unicorn. Meanwhile, Warfarin’s been sitting in the back of the pharmacy for 70 years, cheap, reliable, and paired with a nurse who knows your name.
Also, the JAMA study? Great. But real life isn’t a clinical trial. People forget pills. People take ibuprofen. People eat spinach and then panic. DOACs are great on paper - until your aunt bleeds out and the hospital doesn’t have Praxbind because the budget got cut last quarter.
And don’t even get me started on the cost. I work in a clinic. I’ve had patients cry because they’re choosing between their anticoagulant and their insulin. No one talks about that. The data doesn’t care. But real people? They care. A lot.
laura manning
January 14, 2026 AT 12:42It is imperative to note, with rigorous attention to pharmacokinetic and pharmacodynamic parameters, that the comparative efficacy profiles of direct oral anticoagulants (DOACs) versus vitamin K antagonists (VKAs) are not universally superior across all patient subpopulations. Specifically, in the context of mechanical valvular heart disease, DOACs are contraindicated, per FDA labeling and ACC/AHA guidelines. Furthermore, renal clearance mechanisms for DOACs render them inappropriate in patients with eGFR <15 mL/min, whereas Warfarin’s hepatic metabolism confers a distinct advantage in end-stage renal disease. The cost differential, while substantial, must be contextualized within the broader framework of healthcare system sustainability and equitable access.
Jay Powers
January 16, 2026 AT 12:25Both have their place. Warfarin’s old but it’s like a reliable truck - you know how to fix it. DOACs are like a Tesla - sleek, quiet, no oil changes, but if the battery dies and you’re miles from a charger? You’re stuck. The real issue isn’t the drugs. It’s that we don’t have the infrastructure to support the new ones. Not every hospital can afford Praxbind. Not every patient can afford the pill. We need better access, not just better science.
Lawrence Jung
January 17, 2026 AT 06:44It’s funny how we romanticize progress. DOACs are just corporate marketing dressed up as medicine. Warfarin worked for decades. Now we’ve got this expensive, fragile system built on proprietary drugs and hospital stockpiles that no one can afford. We’re not advancing health. We’re just making the rich healthier and the poor gamble with their lives.
Alice Elanora Shepherd
January 17, 2026 AT 11:23One thing rarely mentioned: patient adherence. DOACs require strict timing - once or twice daily, no skipping. Warfarin? You can be a bit more flexible, especially if you’re on a stable dose. For elderly patients, especially those with memory issues, that matters. I’ve seen more hospitalizations from missed DOAC doses than from Warfarin fluctuations. It’s not just about efficacy - it’s about what people can actually do, day after day.
Christina Widodo
January 18, 2026 AT 20:55Wait - so if someone has a bleed and they’re on a DOAC and the hospital doesn’t have the antidote, what do they actually do? Just give PCC and hope? Is there any data on survival rates in that scenario? I feel like this is the elephant in the room.
Cassie Widders
January 20, 2026 AT 19:26My uncle’s on Warfarin. He hates the blood tests. But he says he’d rather have the routine than risk dying because the hospital ran out of the fancy antidote. Simple as that.
Jay Powers
January 22, 2026 AT 07:15That’s exactly right. And that’s why I tell patients: it’s not about which drug is better on paper. It’s about which one you can live with. If you’re going to miss doses because it’s too expensive, or you’re too scared because the reversal agent might not be there - then Warfarin might be the safer choice, even if it’s more work. Medicine isn’t just science. It’s survival.