When a generic medication fails to control your condition, insurance denials are common - but not final. Learn how to fight back with documented evidence, physician support, and proven appeal strategies that work.
MoreTherapeutic Inequivalence: When Generic Drugs Don't Work the Same
When a generic drug is labeled therapeutic equivalence, a regulatory status meaning it performs the same way as the brand-name version in the body. Also known as bioequivalence, it's supposed to guarantee that switching from a brand to a generic won't change your outcome. But therapeutic inequivalence, the gap between expected and actual performance happens more often than most patients realize—especially with combination pills, sensitive conditions, or complex drug interactions.
It’s not always about the active ingredient. The real trouble often comes from inactive ingredients, fillers, dyes, or coatings that affect how the drug is absorbed. For example, a generic version of a combination blood pressure pill might use a different binder that slows absorption just enough to make your control worse. Or an anti-nausea drug like ondansetron might work fine for most people, but if your body processes it differently due to a minor formulation change, you could end up vomiting anyway. These aren’t mistakes—they’re legal variations allowed under current rules. But for someone with epilepsy, heart rhythm issues, or chronic pain, even small shifts can mean hospital visits or failed treatments.
Pharmacists are often allowed to swap medications under therapeutic interchange, a practice where one drug is replaced with another deemed similar. But not all swaps are equal. A drug that works for one person might fail for another simply because of how the body reacts to a new coating or release mechanism. The FDA tracks these issues through deficiency letters and post-market reports, but patients rarely see the data. What you do see are warning icons on labels, unexpected side effects, or sudden drops in effectiveness—all signs something’s off.
And it’s not just about pills. With drugs like antimalarials, corticosteroids, or even common NSAIDs, small changes in formulation can trigger dangerous interactions—especially when combined with other meds. If you’re on multiple drugs, have a chronic condition, or notice your symptoms changing after a refill, it’s not just in your head. The system assumes all generics are interchangeable. But biology doesn’t care about labels—it cares about what actually gets into your bloodstream.
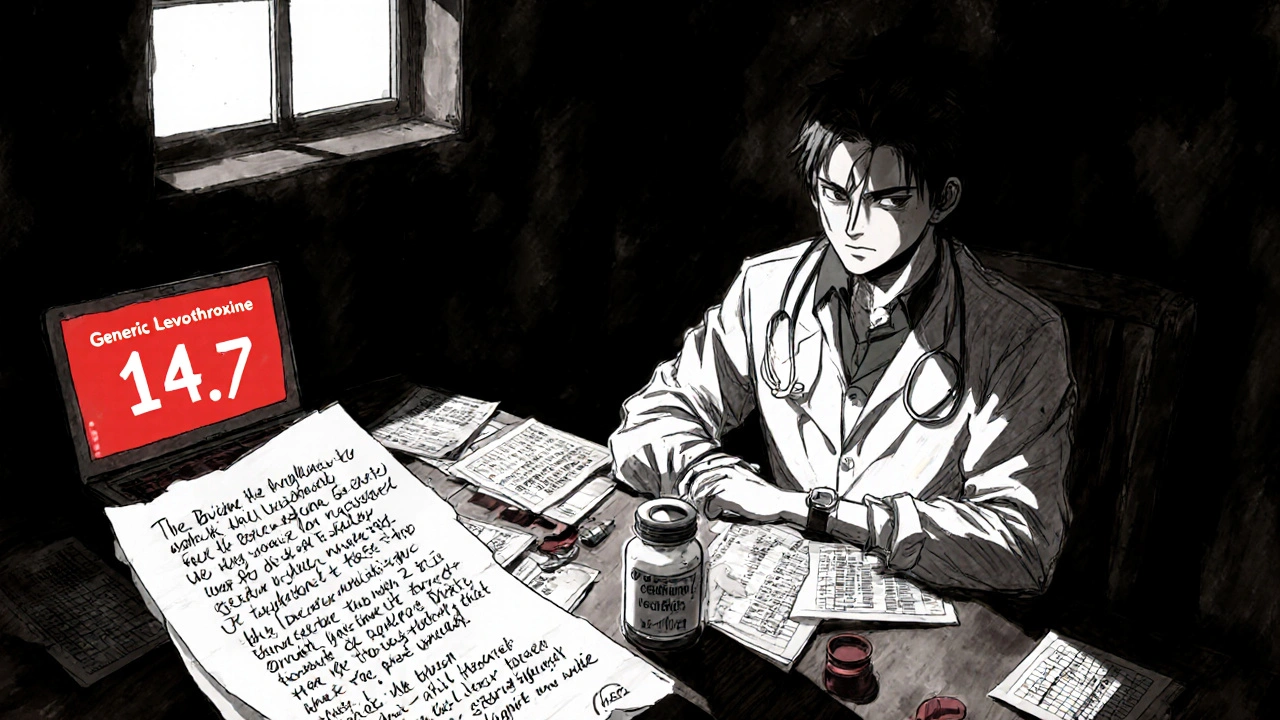
Below, you’ll find real cases where people ran into these exact problems: a generic combination drug that caused nausea, a thyroid pill that stopped working after a switch, a heart medication that led to irregular rhythms because of a coating change. These aren’t rare exceptions. They’re symptoms of a system built on averages, not individual biology. If you’ve ever wondered why your meds suddenly stopped working—or started causing new problems—this collection will show you why, and what to do next.