Learn why corticosteroids cause high blood sugar, who’s at risk, and how to monitor and treat steroid‑induced hyperglycemia effectively.
MoreCorticosteroids and Hyperglycemia Management: What You Need to Know
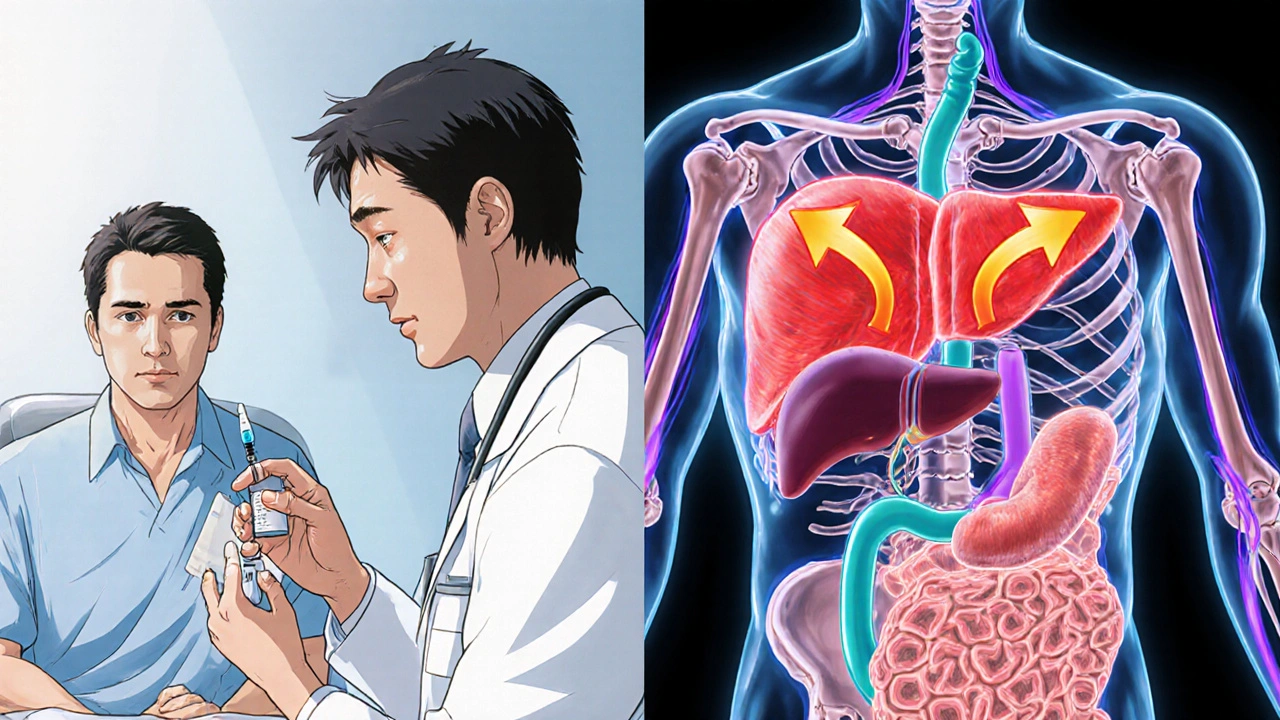
When you take corticosteroids, a class of anti-inflammatory drugs used for conditions like asthma, rheumatoid arthritis, and autoimmune disorders. Also known as glucocorticoids, they work by calming your immune system—but they also mess with how your body handles sugar. That’s why many people on long-term corticosteroid therapy end up with high blood sugar, sometimes even developing steroid-induced diabetes. It’s not a side effect you can ignore. If you’re on these meds, managing your blood sugar isn’t optional—it’s part of your treatment plan.
Hyperglycemia from corticosteroids doesn’t happen the same way for everyone. Some people see their numbers climb within days; others take weeks. The higher the dose and the longer you take it, the worse it gets. Prednisone, dexamethasone, methylprednisolone—they all do this. It’s not about being lazy or eating too much sugar. These drugs make your liver pump out more glucose and block insulin from doing its job. Your body thinks it’s under stress, so it hoards sugar for energy—even when it doesn’t need it.
That’s why hyperglycemia management, the process of keeping blood sugar levels stable while on corticosteroids is so critical. It’s not just about popping a metformin pill and calling it a day. You need a plan. That means checking your blood sugar more often—sometimes four times a day. It means adjusting your meals: fewer refined carbs, more fiber, consistent timing. It means talking to your doctor about whether your steroid dose can be lowered or switched to a local form (like an inhaler or cream) if possible. And if you’re already diabetic? Your insulin or oral meds might need a serious tweak.
Some people think this is just a temporary problem. It’s not always. Even after stopping corticosteroids, blood sugar can stay high for weeks. And if you’ve had steroid-induced hyperglycemia once, you’re more likely to see it again if you need these drugs in the future. That’s why knowing your baseline numbers before starting treatment matters. Write them down. Track changes. Tell your doctor if your energy drops, you’re thirsty all the time, or you’re peeing more than usual. These aren’t minor annoyances—they’re red flags.
And it’s not just you. Your care team needs to be on the same page. Endocrinologists, pharmacists, and your primary doctor should all know you’re on steroids. That way, they can coordinate your care instead of treating each problem separately. This isn’t just about sugar—it’s about preventing complications like nerve damage, kidney stress, or infections that heal slower when blood sugar is up.
Below, you’ll find real-world advice from people who’ve been there. Some posts show how to adjust diet and activity to keep sugar in check. Others compare medications used to treat steroid-induced hyperglycemia. There’s even a guide on how to talk to your doctor about reducing steroid doses without risking a flare-up. You won’t find fluff here. Just clear, practical steps you can use right away—whether you’re managing this for yourself or helping someone you care about.