20
Feb

When you need a steady supply of blood pressure pills, diabetes meds, or antidepressants, mail-order generics sound like a dream: mail-order generics delivered to your door, often for less than what you’d pay at the corner pharmacy. But behind the convenience and low copays lies a system full of gaps - some that could cost you more than money.
How Mail-Order Generics Actually Work
Mail-order pharmacies don’t just ship pills. They’re part of a larger system tied to your insurance plan’s pharmacy benefit manager (PBM). Most plans let you get a 90-day supply instead of a 30-day one, which cuts down on trips to the pharmacy and sometimes lowers your out-of-pocket cost. For example, a 90-day supply of a generic blood pressure drug might cost you $10 with insurance, while the same drug at a retail pharmacy could be $45. But here’s the catch: that $10 isn’t the real price. It’s a copay - a fixed fee you pay, while your insurer and PBM negotiate the rest. What you don’t see is how much the pharmacy is actually being paid. A 2023 analysis by The Happy PharmD found that a generic antidepressant costing $12 at a retail pharmacy was billed to insurers at $100 through mail-order - an 800% markup. Brand-name drugs? Sometimes 35 times more than retail. The system works best for chronic conditions. If you take the same pills every day for years, mail-order makes sense. About 58% of diabetes patients and 63% of people with high blood pressure use it, according to IQVIA. But if you need an antibiotic for a sudden infection or an inhaler for a flare-up? Forget it. Mail-order isn’t built for urgency.The Real Cost Savings - And Where They Disappear
Yes, many people save money. One user on GoodRx said they cut $45 a month by switching to mail-order for their hypertension meds. For retirees on Medicare Part D, nearly one in three uses mail-order. That’s because the program pushed adoption back in 2006, and PBMs have kept pushing it since. But savings aren’t universal. Uninsured patients? They’re often stuck paying full price - sometimes $500 a month for drugs like semaglutide or tirzepatide. And even insured people can get hit with surprise costs if their plan doesn’t cover the mail-order pharmacy they’re using. Some plans only offer discounts if you use their preferred pharmacy. If you don’t, you might pay more than if you’d just walked into a local drugstore. Also, not all generics are created equal. Mail-order pharmacies don’t always carry every generic version. If your doctor prescribed a specific brand of generic metformin and the mail-order pharmacy only stocks another, you might get a different pill - same active ingredient, but different shape, color, or filler. That’s not a safety issue per FDA rules, but it can confuse patients. One study found people switching between generic versions of topiramate ended up with more hospital visits - likely because they got confused, skipped doses, or didn’t recognize their meds.Temperature Chaos: When Your Pills Go Bad
Think your insulin or thyroid meds are safe in a box shipped across the country? Think again. Medications need to stay between 68°F and 77°F during transit. Too hot? Too cold? They lose potency. Insulin, for example, starts breaking down after 24 hours above 86°F. A 2023 study in the Journal of the American Pharmacists Association found that only one-third of mail-order shipments stayed within that safe range. Reddit threads are full of horror stories: insulin shipped in summer heat, arriving melted. Thyroid pills exposed to freezing temperatures on a porch. One patient in Texas lost three months’ supply of levothyroxine after a delivery truck sat in 100°F heat for hours. The FDA has logged over 1,200 reports of temperature-related failures between 2020 and 2023. Experts say the real number is likely much higher - most people don’t report it. There are no federal rules requiring temperature monitoring, packaging standards, or delivery tracking for meds. Only one company, Express Scripts, has publicly committed to using cold packs and insulated packaging for sensitive drugs. The rest? It’s a gamble.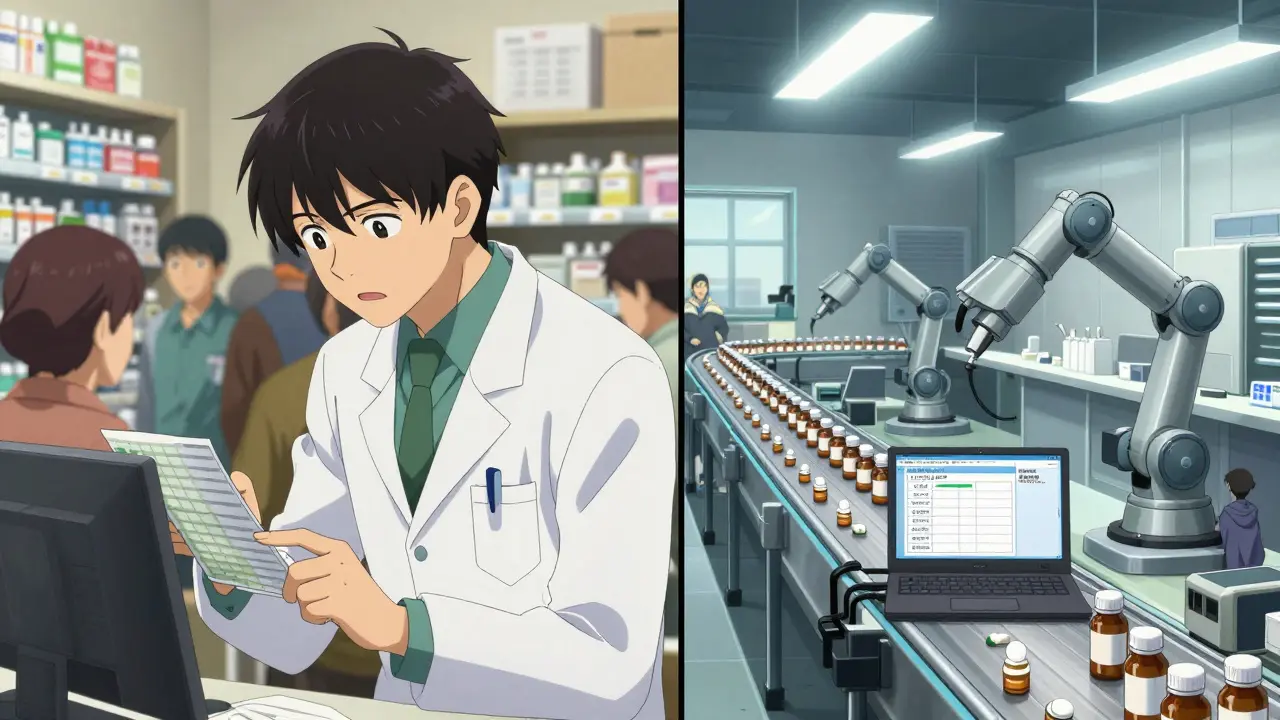
Missing the Pharmacist: A Silent Risk
At your local pharmacy, the pharmacist asks: “Are you taking anything else?” “Any new symptoms?” “Did you have trouble with this before?” At a mail-order pharmacy? You get a label and a tracking number. A 2023 Consumer Reports survey found 68% of users worried about missing those face-to-face checks. Pharmacists catch drug interactions, duplicate prescriptions, and dangerous combinations. A patient on warfarin and a new antibiotic? A local pharmacist would flag it. A mail-order system might not even know the patient is on both - especially if they’re filling one script at CVS and another through mail-order. And when something goes wrong? You can’t walk up to the counter. You call a 1-800 number. Wait on hold. Get transferred. Hope someone remembers your name. For older adults or people with cognitive issues, this isn’t just inconvenient - it’s dangerous.Who Benefits? Who Gets Left Behind?
The big players - Express Scripts, CVS Caremark, OptumRx - control nearly 80% of the mail-order market. They’re owned by giant insurers and health corporations. Their goal isn’t to improve your health. It’s to maximize profit. The numbers tell the story: mail-order sales jumped from $86 billion in 2013 to over $206 billion in 2023. Prescription volume? Up just 11%. That means prices, not volume, drove growth. And the people paying? Mostly you. Medicare beneficiaries? They’ve been pushed into mail-order for decades. Younger adults? Often not even offered the option unless they’re on an employer plan that mandates it. The uninsured? They’re priced out. The system works best for those with stable insurance and predictable meds. Everyone else? They’re left navigating a maze of hidden costs, unreliable deliveries, and no one to ask for help.
How to Use Mail-Order Generics Safely
If you’re using mail-order, here’s how to protect yourself:- Order early - At least two weeks before you run out. Delays happen.
- Check the packaging - If pills are discolored, melted, or smell odd, don’t take them. Call the pharmacy. File a report with the FDA.
- Know your pharmacy - Use your insurer’s preferred network. Otherwise, you might pay more.
- Keep a list - Track every medication you take, including over-the-counter ones. Share it with your doctor and pharmacist.
- Ask about temperature control - If you take insulin, epinephrine, or other sensitive drugs, ask if the pharmacy uses cold packs and insulated shipping. If they say no, find another option.
- Don’t mix and match - If you’re using both retail and mail-order, ask your primary pharmacist to review all your meds. They can spot dangerous interactions.
