
When you get a CT scan or X-ray with contrast dye, most people don’t think twice about it. But for some, that same procedure can trigger a dangerous reaction. These aren’t just minor rashes or nausea-they can be life-threatening. The good news? We know how to prevent them. And the key isn’t just giving medicine before the scan. It’s knowing who needs it, when to give it, and what to do if things go wrong.
What Are Contrast Dye Reactions?
Contrast dye-usually iodinated-is used to make blood vessels, organs, and tissues show up clearly on CT scans and some X-rays. It’s not a drug you take for a cold or infection. It’s a one-time injection, and most people handle it just fine. But about 0.04% to 0.22% of people have some kind of reaction. Severe reactions? That’s rarer-around 0.01% to 0.04%. Still, even one severe reaction is one too many.
Reactions fall into two categories: allergic-type (immediate) and non-allergic (delayed). The ones we worry about most are the immediate ones. These can happen within minutes and include hives, swelling, trouble breathing, low blood pressure, or even cardiac arrest. They’re not true allergies like peanut or bee sting reactions. They’re more like a chemical shock to the body. That’s why calling them "allergies" is misleading. But we still treat them like emergencies.
Who Needs Premedication?
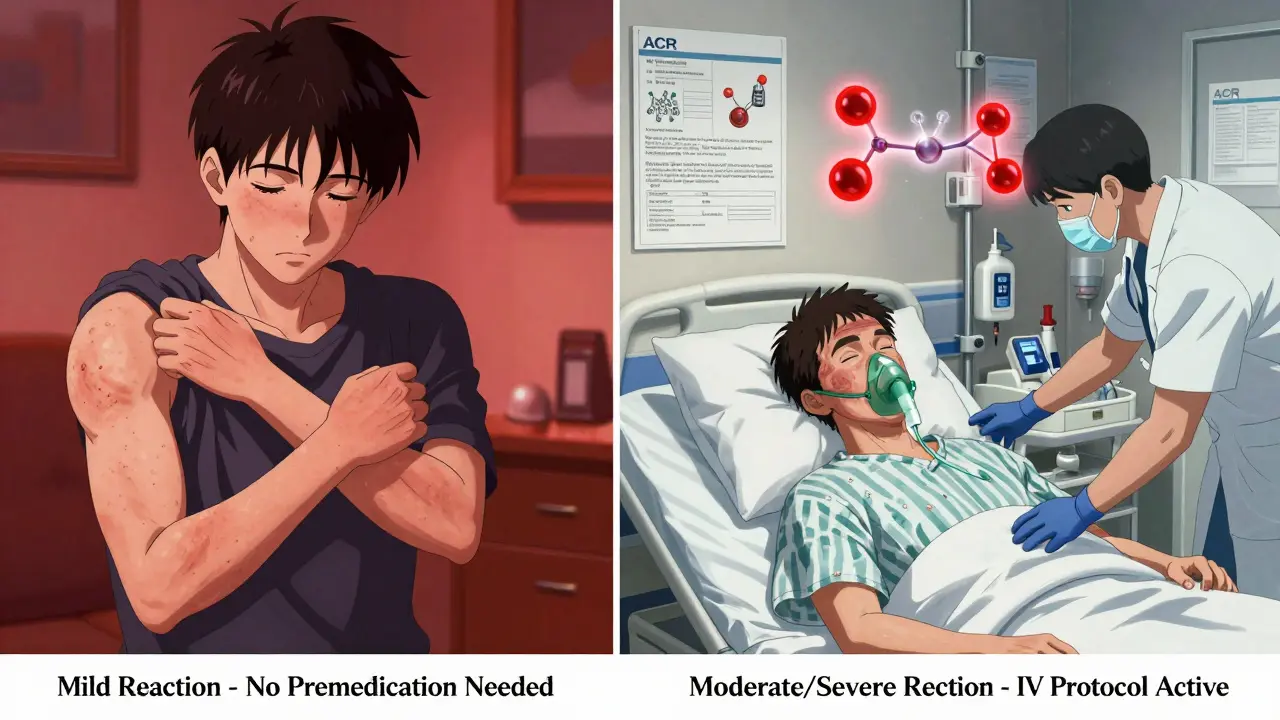
Not everyone who’s had a reaction before needs to be premedicated. The rules have changed. A mild reaction-like a little itching or a small rash-doesn’t automatically mean you’re at high risk. Studies from UCSF and Yale show that if you had a mild reaction in the past, your chance of having another one is very low. No premedication needed.
But if you’ve had a moderate reaction-think swelling of the face or throat, vomiting, wheezing, or a drop in blood pressure-you’re in a higher-risk group. And if you’ve had a severe reaction-like cardiac arrest, respiratory failure, or loss of consciousness-you’re in the danger zone. In most cases, doctors will avoid contrast dye altogether unless it’s absolutely necessary.
Here’s something most people get wrong: having a shellfish allergy, iodine allergy, or reacting to Betadine doesn’t mean you’ll react to contrast dye. That’s a myth. Studies show people with those allergies have only a 2- to 3-fold higher risk than someone with no history at all. That’s not enough to justify premedication. You don’t need to avoid seafood before a CT scan.
The Standard Premedication Protocols
If you’re in the high-risk group, premedication is your safety net. But it’s not one-size-fits-all. There are two main approaches: oral and IV.
Oral protocol (for outpatient settings):
- Prednisone 50 mg by mouth at 13 hours, 7 hours, and 1 hour before the scan
- Diphenhydramine (Benadryl) 50 mg by mouth 1 hour before the scan
This is the classic 13-hour schedule used at places like Dartmouth-Hitchcock and UCLA. The prednisone is a steroid that calms down your immune system. The Benadryl blocks histamine, which causes swelling and itching. But Benadryl makes you sleepy. Really sleepy. So if you’re on this schedule, you must have someone drive you home. No exceptions.
IV protocol (for inpatients and emergencies):
- Methylprednisolone (Solu-Medrol) 40 mg IV, then every 4 hours until scan time
- OR hydrocortisone (Solu-Cortef) 200 mg IV, then every 4 hours until scan time
- Diphenhydramine 50 mg IV 1 hour before the scan
This version works faster. It’s used when you’re already in the hospital or when the scan can’t wait. IV meds hit your system right away. No waiting 13 hours. But you still need the Benadryl an hour before.
The 5-Hour Shortcut
What if you need a scan tomorrow and can’t wait 13 hours? There’s a faster option. A 2017 study in Radiology by Dr. Behrang Mervak compared the old 13-hour plan with a 5-hour version: methylprednisolone 32 mg by mouth at 5 hours and again at 1 hour before the scan, plus Benadryl 50 mg at 1 hour. The results? Just as effective.
That’s huge. Now, if you’re in the ER or your doctor schedules you last minute, you don’t have to cancel the scan. You can still be protected. Many hospitals have switched to this accelerated protocol for urgent cases. It’s not yet universal, but it’s gaining ground fast.
What About Kids?
Pediatric dosing is different. You can’t just give a child half a pill. UCSF recommends cetirizine (Zyrtec) 10 mg by mouth 1 hour before the scan for kids 6 and older. It’s non-sedating, so no driver needed. For younger kids, the protocol is less clear, and doctors often avoid contrast unless absolutely necessary.
What Happens After Premedication?
Even if you take all the right pills, you’re not 100% safe. About 2% of people who are premedicated still have a reaction. That’s called a "breakthrough" reaction. It’s rare, but it happens. That’s why every facility that does contrast scans must be ready.
UCLA, UCSF, and Mount Sinai all require that patients with a history of severe reactions get scanned in places with immediate access to emergency teams. That means crash carts, oxygen, epinephrine, and trained staff within seconds. No rural clinic without an ER nearby should be doing contrast scans on high-risk patients.
And if you’re having a severe reaction? You need to be in a hospital or emergency department. No outpatient imaging center should be handling this alone. Yale’s rule is simple: "The clinical provider should accompany the patient to the radiology suite." That means your doctor or nurse walks with you into the scan room. Just in case.

Switching Contrast Agents
Here’s something surprising: sometimes, the best protection isn’t medicine at all. It’s switching to a different brand of contrast dye.
Not all iodinated contrast dyes are the same. Even if you reacted to one, you might be fine with another. The ACR and Yale both say: if you know which dye caused the problem, switch to a different one in the same class. That can be just as effective as premedication-without the steroids and antihistamines.
Doctors are starting to realize this. In fact, the upcoming ACR Manual Version 11 (expected late 2024) is expected to push this idea even harder. It might become the new standard.
Cost and Real-World Use
Premedication isn’t expensive. Prednisone 50 mg? About 25 cents. Benadryl 50 mg? Fifteen cents. Even if you need three doses of prednisone, you’re looking at under a dollar. Compared to a CT scan that costs $500 to $1,500, it’s a drop in the bucket.
Most academic hospitals follow these protocols exactly. That’s because they’re backed by the American College of Radiology (ACR) Manual on Contrast Media, Version 10.3. But community hospitals? Only about 78% follow them. That gap matters. A patient in a small clinic might not get the right prep-or any prep at all.
What You Should Do
If you’ve ever had a reaction to contrast dye:
- Tell your doctor before scheduling any scan
- Be specific: What happened? Was it mild (itching) or severe (trouble breathing)?
- Ask: "Can we switch to a different contrast agent?"
- If premedication is recommended, ask: "Do I need the 13-hour or 5-hour schedule?"
- Never skip the driver if Benadryl is involved
- Make sure the imaging center knows your history ahead of time
The goal isn’t to scare you. It’s to make sure you get the scan you need-safely. Contrast dye saves lives. But only if we use it wisely.
Do I need premedication if I had a mild reaction to contrast dye in the past?
No, not usually. Studies show that people who had only mild reactions-like a small rash or slight itching-have a very low chance of reacting again. Most guidelines, including those from UCSF and Yale, now recommend skipping premedication for mild reactions. The risk isn’t high enough to justify taking steroids and antihistamines.
Is shellfish allergy a reason to avoid contrast dye?
No. Shellfish allergies are unrelated to iodinated contrast reactions. The myth comes from both containing iodine, but that’s misleading. Your immune system reacts to proteins in shellfish, not iodine. Studies show people with shellfish allergies have only a 2- to 3-fold higher risk of reacting to contrast dye-far below the threshold for routine premedication. You don’t need to avoid seafood before a CT scan.
Can I drive myself home after premedication with Benadryl?
No. Diphenhydramine (Benadryl) causes significant drowsiness, even at standard doses. Most hospitals require you to have a driver if you receive Benadryl before a scan. If you don’t have someone to drive you, the appointment will be rescheduled. Safety comes first-no exceptions.
How long before a scan should premedication start?
Traditional protocols require 13 hours, but a faster 5-hour option is now widely accepted. For oral premedication, prednisone is given at 5 hours and again at 1 hour before the scan. IV regimens can be given as soon as 4-5 hours before. Any regimen started less than 4 hours before the scan is not effective. Timing matters-don’t wait until the last minute.
Are there alternatives to premedication for patients with contrast allergies?
Yes. The best alternative is switching to a different brand of iodinated contrast dye. If you reacted to one type, your doctor may choose another from the same class. Studies show this can be just as effective as premedication. In fact, the upcoming ACR guidelines are expected to prioritize agent switching over routine steroid use. It’s a simpler, safer option when possible.
What if I have a severe reaction during the scan even after premedication?
Even with premedication, about 2% of patients still have a reaction. That’s why imaging centers must be prepared. They need immediate access to emergency equipment: epinephrine, oxygen, IV fluids, and trained staff. If you have a history of severe reactions, you should only be scanned in a hospital or emergency department-not an outpatient clinic. Staff should be ready to act within seconds.
Do I need premedication if I’m getting a CT scan in the emergency room?
Yes-if you have a history of moderate or severe reactions. In emergencies, IV premedication is used because it works faster. Methylprednisolone 40 mg IV and diphenhydramine 50 mg IV are given just before the scan. The scan should still be done in a hospital setting, with your provider nearby in case of reaction. Speed and safety go hand in hand.
Is premedication covered by insurance?
Yes. The medications used-prednisone, methylprednisolone, and diphenhydramine-are generic, inexpensive, and routinely covered. Even with high-deductible plans, the cost is minimal, usually under $1. Insurance typically covers premedication when it’s medically necessary, as documented by your doctor and radiologist.
Can I take my premedication pills the night before?
It depends on the schedule. For the 13-hour protocol, you take the first dose 13 hours before, which often means the night before. But for the 5-hour protocol, you take the first dose only 5 hours before. Taking it too early won’t help. Always follow your provider’s exact timing. Missing a dose or taking it too soon can reduce effectiveness.
What if I forget to take my premedication?
If you miss a dose, call your doctor or the imaging center immediately. If you missed the steroid entirely, the scan may be delayed or canceled-especially if you have a history of severe reactions. If you only missed the Benadryl, they may give it IV in the imaging suite. Never assume you’re still protected. Timing is critical.
