Learn why corticosteroids cause high blood sugar, who’s at risk, and how to monitor and treat steroid‑induced hyperglycemia effectively.
MoreInsulin Resistance and Steroids: How They Connect and What You Need to Know
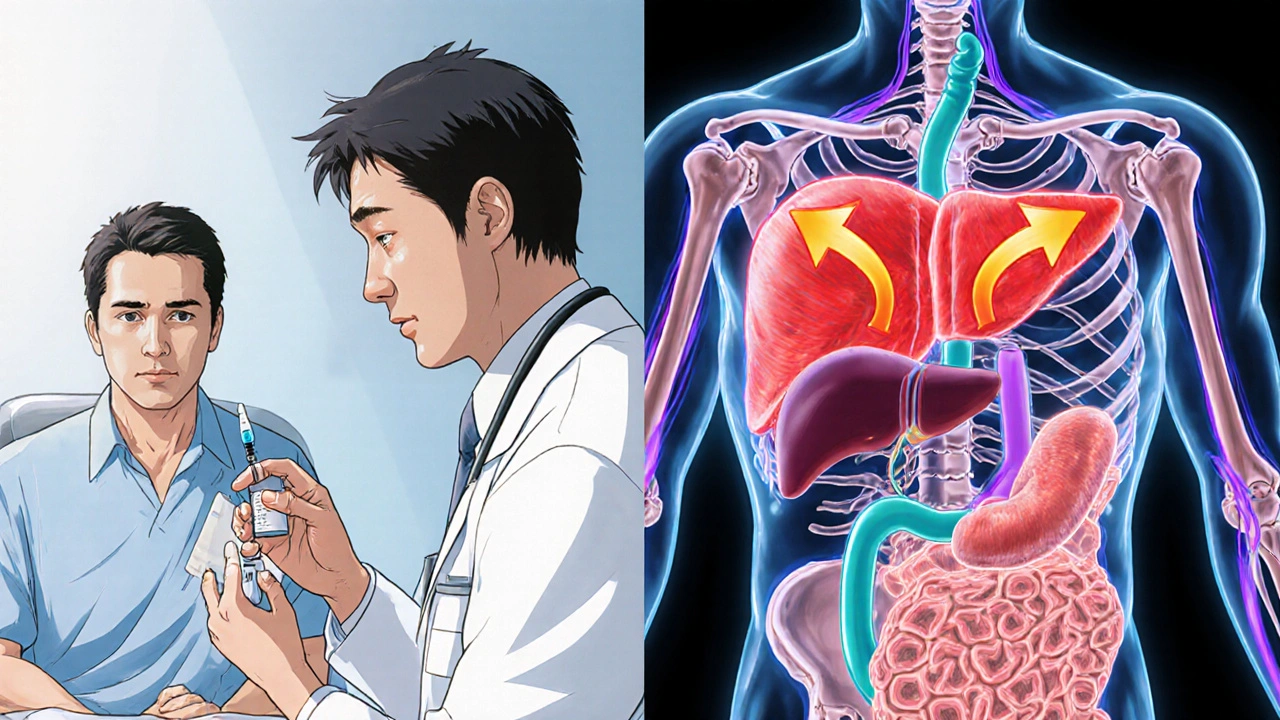
When you take steroids, synthetic hormones that mimic cortisol, often prescribed for inflammation or autoimmune conditions. Also known as corticosteroids, they can sharply raise blood sugar and make your body less responsive to insulin. This isn’t just a side effect—it’s a well-documented metabolic shift that can turn someone with normal glucose levels into someone with prediabetes in weeks. If you’re on long-term steroid therapy, whether for asthma, rheumatoid arthritis, or after an organ transplant, insulin resistance isn’t something you can ignore.
Insulin resistance, a condition where muscle, fat, and liver cells don’t respond properly to insulin, forcing the pancreas to pump out more. Also known as prediabetes, it’s the main driver behind type 2 diabetes. Steroids worsen it by increasing glucose production in the liver and blocking insulin’s ability to move sugar into cells. It’s not about eating too much sugar—it’s about how your body handles it when steroids are in the picture. People who already have risk factors—like being overweight, inactive, or with a family history of diabetes—are hit hardest. But even healthy people can develop temporary insulin resistance while on high-dose steroids.
What makes this worse is that many don’t realize the connection. A patient on prednisone for a flare-up might see their fasting glucose jump from 85 to 130 and think it’s just stress. But it’s the drug. And if left unchecked, this can lead to permanent damage. Monitoring blood sugar isn’t optional—it’s essential. Doctors often recommend checking levels daily during steroid treatment, especially if you’re on more than 20mg of prednisone daily for over two weeks. Some patients need metformin during treatment just to keep glucose in check.
Not all steroids are equal. Inhaled steroids for asthma? Minimal impact on insulin. Topical creams? Almost none. But oral or injected steroids? Big risk. And it’s not just about the dose—it’s about duration. A five-day course might cause a spike, but a three-month course can rewire your metabolism. Even after stopping, it can take months for insulin sensitivity to bounce back. That’s why lifestyle matters: moving more, eating fiber-rich foods, and avoiding refined carbs can help your body recover faster.
You’ll find posts here that dive into how specific drugs like prednisone affect blood sugar, how to tell if steroids are causing your glucose to climb, and what alternatives exist for people who can’t afford the metabolic cost. There’s also advice on managing insulin resistance while still needing steroid treatment—because sometimes, you can’t just quit. This isn’t about fear. It’s about awareness. If you’re on steroids, you deserve to know how they’re changing your body—and what you can do about it.