Learn why corticosteroids cause high blood sugar, who’s at risk, and how to monitor and treat steroid‑induced hyperglycemia effectively.
MoreGlucocorticoid Glucose Control: How Steroids Affect Blood Sugar and What to Do About It
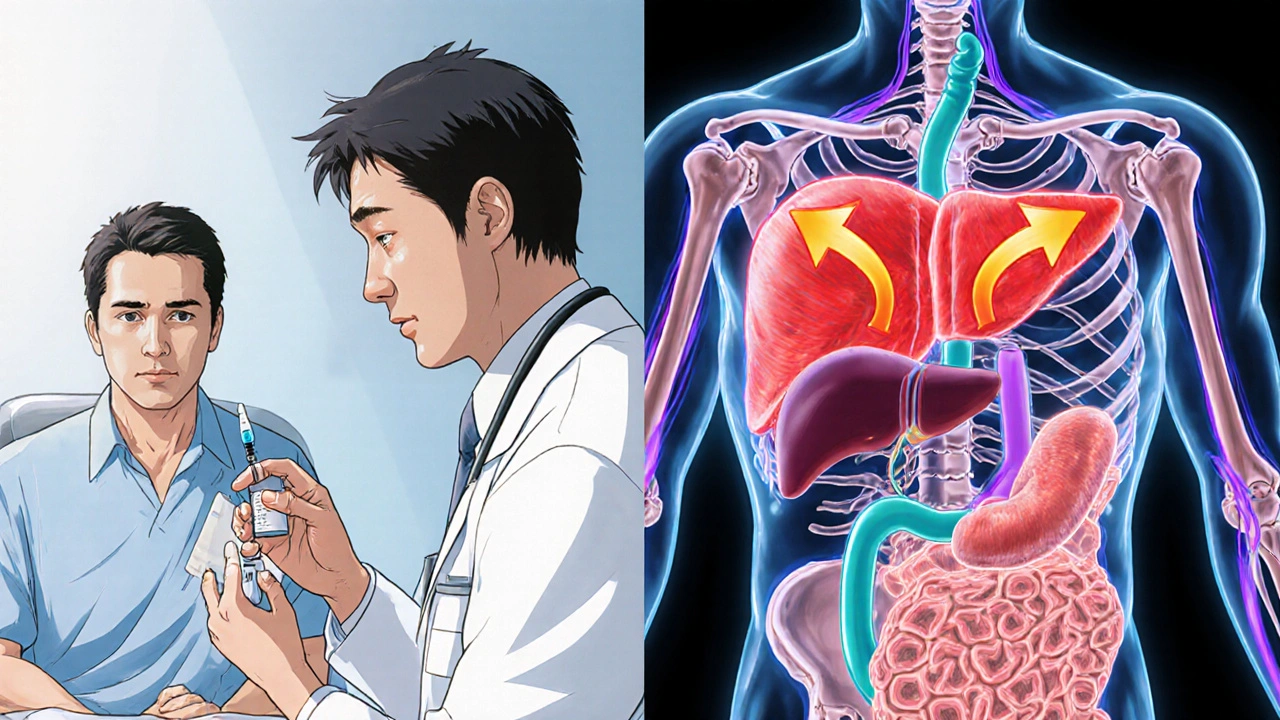
When you take glucocorticoids, a class of steroid hormones used to reduce inflammation and suppress the immune system. Also known as corticosteroids, they’re prescribed for conditions like asthma, rheumatoid arthritis, and autoimmune disorders. But here’s the catch: even short-term use can spike your blood sugar—sometimes dramatically. If you’re diabetic, prediabetic, or just watching your glucose levels, this isn’t just a side effect. It’s a metabolic shift you need to understand and manage.
Glucocorticoids don’t just raise blood sugar. They make your liver dump more glucose into your bloodstream while blocking insulin from doing its job. This is called insulin resistance, a condition where cells stop responding properly to insulin. Your body still makes insulin, but it’s like shouting into a void. The result? High fasting glucose, post-meal spikes, and in some cases, steroid-induced diabetes. This isn’t rare. Studies show up to 30% of people on long-term oral steroids develop elevated glucose levels. Even topical or inhaled forms can cause issues in sensitive individuals.
It’s not just about the dose. Duration matters too. A five-day course of prednisone might give you a temporary spike you can ride out. But if you’re on daily steroids for months? Your body adapts—and your pancreas might struggle to keep up. That’s why people with diabetes on glucocorticoids often need to adjust their meds: more insulin, tighter carb control, or even switching to a different anti-inflammatory drug. And it’s not just adults. Kids on long-term steroids for conditions like nephrotic syndrome show the same pattern: rising glucose, weight gain, and increased risk of metabolic syndrome.
What makes this even trickier is that many people don’t realize their high blood sugar is steroid-related. They blame themselves—"I ate too much," or "I’m not trying hard enough." But the truth? It’s the medicine doing this, not your willpower. The good news? You can fight back. Monitoring glucose more often, timing meals around steroid doses, and working with your doctor to find the lowest effective dose can make a huge difference. Some patients even benefit from metformin during steroid therapy, not to treat diabetes, but to prevent it.
And it’s not just about pills. Inhaled steroids for asthma, nasal sprays for allergies, even joint injections can affect glucose. If you’ve noticed your sugar levels climbing after starting a new steroid treatment, it’s not coincidence. It’s biology. The diabetes, a chronic condition where the body can’t properly regulate blood sugar you didn’t have before might be a side effect you can reverse once the steroid is stopped. But only if you catch it early.
Below, you’ll find real-world comparisons and practical guides from people who’ve been there—whether they’re managing steroid-induced glucose spikes, switching therapies to avoid them, or learning how to balance inflammation control with metabolic health. These aren’t theoretical articles. They’re the kind of insights you need when your doctor says, "Just take this," and you’re left wondering, "But what about my blood sugar?"