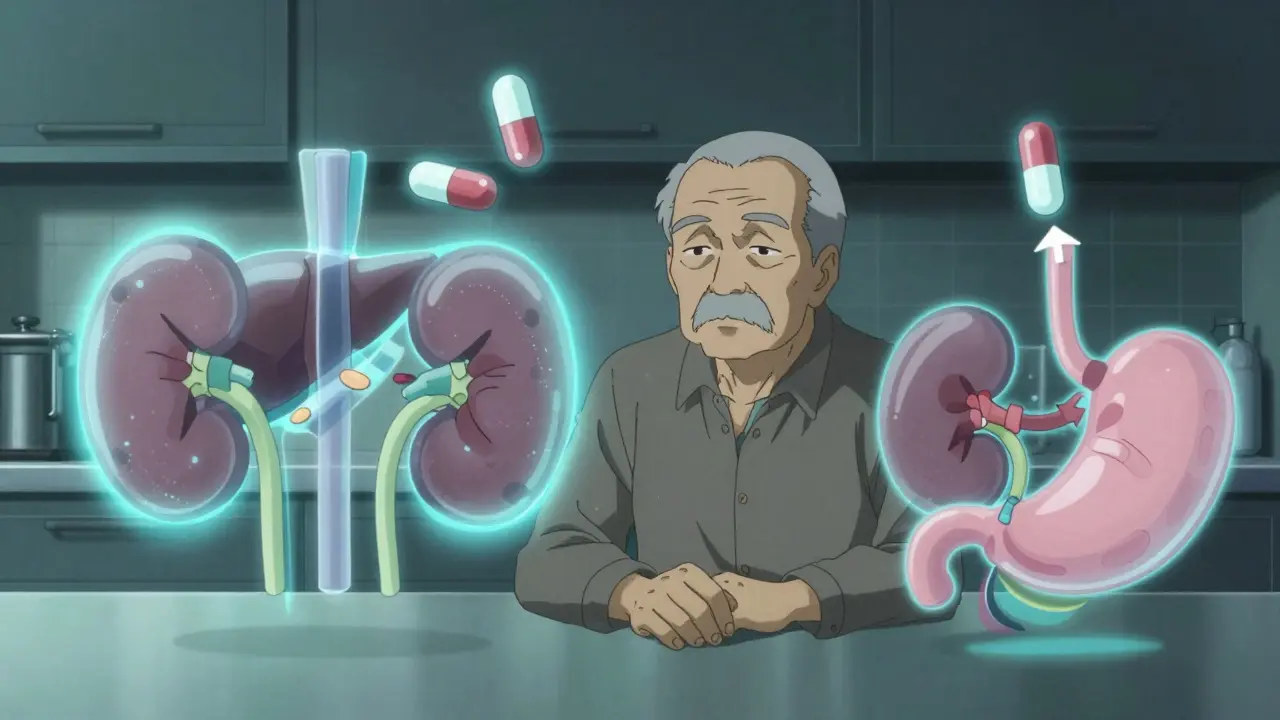
When you’re older, your body doesn’t process medicine the same way it did when you were younger. A pill that worked perfectly at 50 might make you dizzy or sick at 75-not because you’re doing anything wrong, but because your body has changed. This isn’t about being frail or weak. It’s about biology. Your liver, kidneys, stomach, and even your fat distribution shift over time, and those changes directly affect how drugs move through you. Ignoring this can lead to dangerous side effects, hospital visits, or worse. The good news? With the right adjustments, medications can still work safely and effectively. The key is understanding how aging changes your body’s relationship with drugs-and what to do about it.
Why Older Bodies Need Different Doses
Think of your body as a factory that processes everything you take in. In youth, that factory runs at full speed. By the time you hit 65, it’s running at 60-70% capacity. This isn’t a guess-it’s backed by decades of research. According to the American Geriatrics Society a leading authority on geriatric care, which publishes the Beers Criteria®-a widely used guide for safe prescribing in older adults, over 60% of medications require dose changes for adults over 65. The reason? Four key changes happen in your body as you age.
- Absorption slows down. Your stomach produces less acid, and blood flow to your intestines drops by 20-30%. This means some drugs don’t get absorbed as quickly or as completely. For example, the antibiotic amoxicillin may take longer to reach its peak level in your blood.
- Distribution shifts. As you age, you lose muscle and gain fat. Since water-soluble drugs (like digoxin or lithium) hang out in muscle, and fat-soluble ones (like diazepam) get stored in fat, your body’s makeup changes how drugs spread around. A standard dose might end up too concentrated in your bloodstream.
- Metabolism slows. Your liver shrinks and gets less blood flow. It also loses enzymes that break down drugs. Studies show hepatic clearance the liver’s ability to remove drugs from the bloodstream drops by 30-50% for many medications. That means drugs like statins or antidepressants stick around longer, increasing the risk of side effects.
- Excretion declines. Your kidneys filter less. After age 30, your creatinine clearance drops about 8 mL per minute every decade. By 70, many people have less than half the kidney function they had at 25. Drugs cleared by the kidneys-like gabapentin, metformin, or warfarin-can build up to toxic levels if doses aren’t lowered.
A 2022 JAMA Internal Medicine study found that adverse drug events harmful side effects from medications cause 35% of hospital admissions in people over 65. Most of these aren’t accidents-they’re preventable dosing errors.
The "Start Low, Go Slow" Rule
The golden rule in geriatric prescribing isn’t complicated: start low, go slow. It was first formalized in the 1980s and is now standard practice. But what does that actually look like in real life?
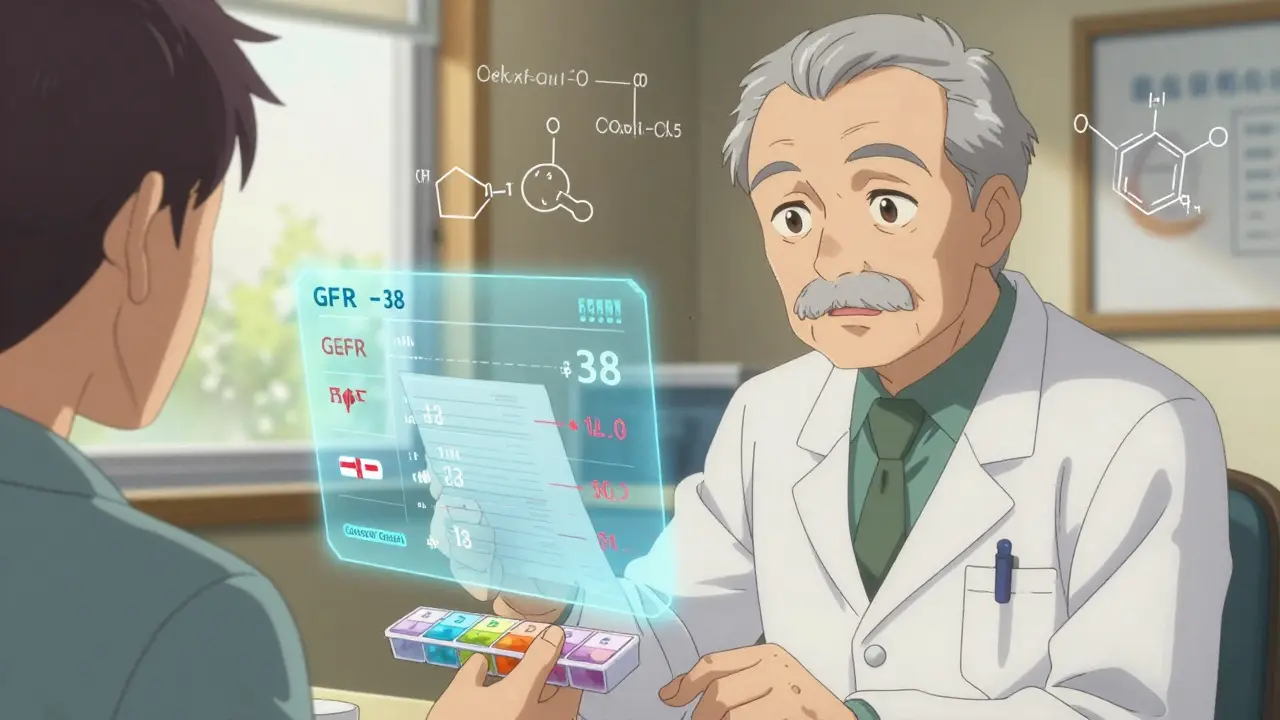
Take metformin a common diabetes drug cleared by the kidneys. For a young adult, the starting dose is usually 500 mg twice daily. For someone over 70 with reduced kidney function, the starting dose is 250 mg once daily. And if their eGFR (a measure of kidney function) is between 30 and 45, the dose stays at 500 mg per day max-never higher. If it drops below 30, the drug is stopped entirely.
Another example: gabapentin used for nerve pain and seizures. The standard adult dose is 300 mg three times a day. For seniors, the initial dose is 100 mg once a day. It’s increased slowly over weeks, if needed. Why? Because it’s eliminated almost entirely by the kidneys. A 75-year-old with normal creatinine levels still needs 40% less than a 40-year-old.
Even blood pressure pills need adjustment. A typical starting dose of lisinopril is 10 mg. For someone over 70, it’s often 2.5 or 5 mg. Why? Older adults are more sensitive to drops in blood pressure, which can cause fainting, falls, or kidney damage.
How Doctors Calculate the Right Dose
It’s not guesswork. Doctors and pharmacists use real formulas to adjust doses. The most common one is the Cockcroft-Gault equation a formula that estimates kidney function using age, weight, and serum creatinine. Here’s how it works:
For men: CrCl = [(140 - age) × weight (kg)] / (72 × serum creatinine)
For women: Multiply the result by 0.85
If your CrCl is below 50 mL/min, most kidney-cleared drugs need a dose reduction. If it’s below 30, many are avoided altogether. This isn’t theoretical-it’s used daily in hospitals and clinics.
For drugs processed by the liver, doctors use the Child-Pugh score a system that rates liver function based on blood tests and symptoms. A score of 7-9 (moderate impairment) means cut the dose in half. A score of 10-15 (severe) means avoid the drug or use only 25% of the normal dose.
Some drugs, like digoxin, have narrow safety margins. In younger adults, the target blood level is 0.8-2.0 ng/mL. In seniors, it’s 0.5-0.9 ng/mL. Too high, and you risk heart rhythm problems. Too low, and it doesn’t work. That’s why therapeutic drug monitoring measuring exact drug levels in the blood matters-but only 15% of medications have this option available.
High-Risk Medications to Watch Out For
The 2023 Beers Criteria® the most updated list of potentially inappropriate medications for older adults lists 30 classes of drugs that are risky for seniors. Here are the top three:
- Benzodiazepines (like lorazepam or diazepam): Increase fall risk by 50%. They cause drowsiness, confusion, and memory issues. Even short-term use can be dangerous.
- NSAIDs (like ibuprofen or naproxen): Raise the risk of stomach bleeding by 300%. They also worsen kidney function and can spike blood pressure. Acetaminophen is often a safer choice for pain.
- Anticholinergics (like diphenhydramine/Benadryl or oxybutynin): Double the risk of dementia with long-term use. They’re still found in many sleep aids and bladder pills-but they’re not worth the cost.
These aren’t just "avoid" drugs-they’re drugs that should be replaced. For example, melatonin or cognitive behavioral therapy can help sleep. Physical therapy and pelvic floor exercises often work better than oxybutynin for bladder issues.
The Polypharmacy Problem
More than half of older adults take five or more prescription drugs. That’s called polypharmacy. It’s not inherently bad-if each drug is necessary. But when prescriptions pile up, interactions and dosing errors multiply.
A 2016 JAMA Internal Medicine study found that 55% of U.S. adults over 65 take at least five prescription medications. Each additional drug increases the risk of a harmful interaction. Warfarin, for example, interacts with over 100 other medications. A simple antibiotic can spike your INR (a measure of blood thinning) and cause dangerous bleeding.
That’s why medication reviews a structured process to check if all drugs are still needed and properly dosed are critical. The Medication Appropriateness Index (MAI) a 10-question tool that scores how appropriate each drug is for an older patient is one of the best tools for this. A score above 18 means at least one drug is inappropriate and should be adjusted or stopped.
Pharmacists who specialize in geriatrics reduce medication errors by 67%. That’s not magic-it’s expertise. They spot interactions, check kidney and liver function, and know which doses are too high.
What You Can Do
You don’t need to be a doctor to help manage your meds. Here’s what works:
- Bring all your meds to every appointment. This is called a "brown bag review." Include pills, supplements, and over-the-counter drugs. Many people forget their aspirin or herbal teas-both can interact.
- Ask: "Is this still necessary?" Just because you’ve been on a drug for years doesn’t mean you still need it. Ask your doctor if any can be stopped or lowered.
- Know your kidney numbers. Ask for your eGFR and creatinine clearance. If you don’t know them, you can’t know if your dose is right.
- Use a pill organizer. Weekly blister packs cut errors by 40%. Pharmacies can prepare them for you.
- Involve a family member. Studies show caregiver involvement improves adherence by 37%. Have someone help you check doses or call the pharmacy.
Electronic health records now flag risky dosing. If your doctor sees a warning about a high dose for your age or kidney function, it’s not a mistake-it’s a lifesaver.
What’s Changing Now
The field is evolving fast. The FDA now requires age-specific data in clinical trials. In 2010, only 28% of trial participants were over 65. By 2022, that jumped to 42%. That’s progress.
Tools like MedAware an AI system that predicts dangerous dosing errors in older patients are now being tested in hospitals. In a 2023 Johns Hopkins pilot, it cut dosing errors by 47%.
Future guidelines will focus less on age and more on function. A 70-year-old who walks fast, remembers their meds, and has strong kidneys might need a full dose. A 65-year-old who struggles to climb stairs and has a CrCl of 40 might need a much lower one. That’s the future: functional age, not calendar age.
By 2030, personalized dosing based on kidney, liver, and cognitive function could become standard for 70% of high-risk drugs. That could prevent over 250,000 hospitalizations each year in the U.S. alone.
Why can’t I just take the same dose I’ve always taken?
Your body changes as you age. Your kidneys filter less, your liver breaks down drugs slower, and your body composition shifts-more fat, less muscle. These changes mean drugs stay in your system longer and can build up to dangerous levels. A dose that was safe at 50 might be toxic at 75.
Are over-the-counter medicines safe for seniors?
Not always. Many OTC drugs are high-risk for older adults. Antihistamines like Benadryl, NSAIDs like ibuprofen, and sleep aids with diphenhydramine can cause confusion, falls, kidney damage, or stomach bleeding. Always check with a pharmacist before taking any OTC drug regularly.
How do I know if my kidney function is low?
Your doctor can check your eGFR (estimated glomerular filtration rate) with a simple blood test. If your eGFR is below 60, your kidneys are not working at full capacity. Below 30 means you need major dose adjustments or to avoid certain drugs entirely. Ask for this number at every visit.
Can I stop taking a medication if I feel fine?
Never stop a prescribed medication without talking to your doctor. But you can ask: "Is this still necessary?" Many seniors take drugs for conditions that have improved or are no longer active. A medication review can help identify drugs you no longer need.
Do pharmacists help with dosage adjustments?
Yes-especially geriatric pharmacists. They specialize in how aging affects drug response. They check for interactions, adjust doses based on kidney and liver function, and help simplify regimens. Many pharmacies now offer free medication reviews. Ask if yours does.
Final Thoughts
Medication isn’t one-size-fits-all-not even close. What worked for you at 40 might hurt you at 70. The goal isn’t to take fewer pills-it’s to take the right ones, at the right dose, for the right reason. With better testing, smarter tools, and more awareness, older adults can stay healthy without being overmedicated. The system is getting better. But you still need to be your own best advocate. Ask questions. Know your numbers. And never assume a dose is safe just because it’s been years since you started it.
