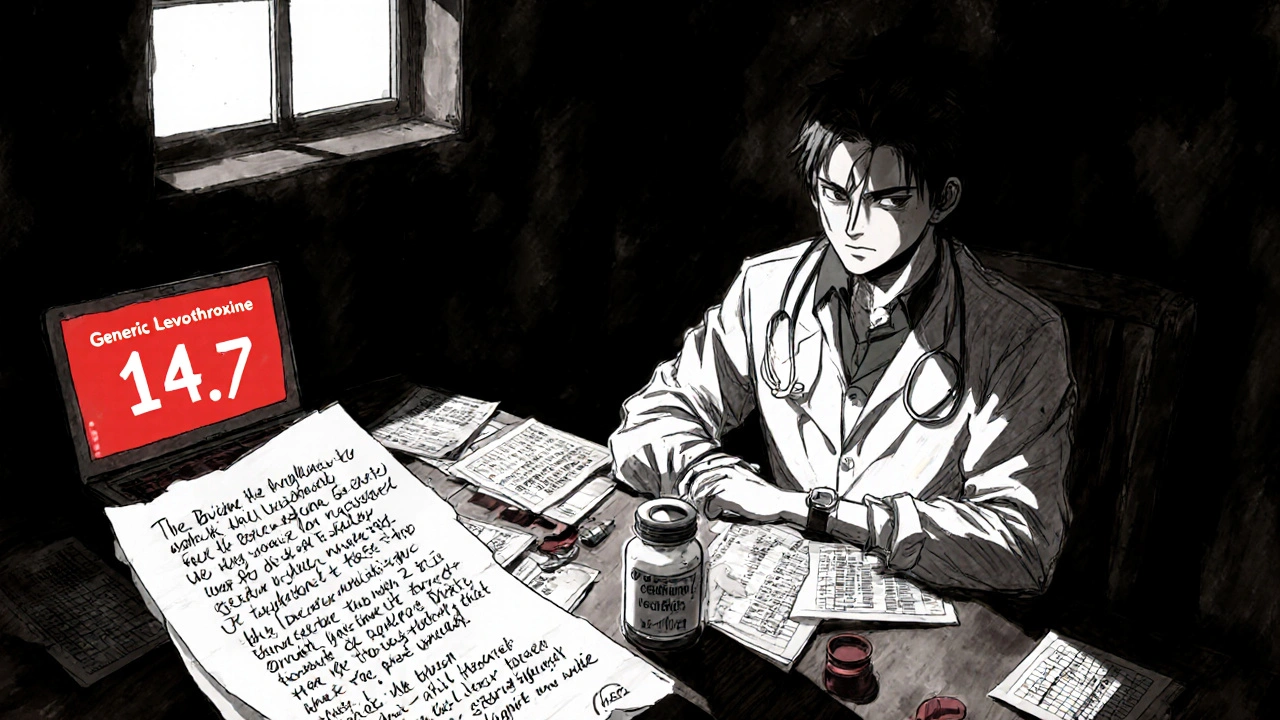
When a generic medication fails to control your condition, insurance denials are common - but not final. Learn how to fight back with documented evidence, physician support, and proven appeal strategies that work.
MoreBrand-Name Drug Approval: How Drugs Get Approved and What Happens Behind the Scenes
When you pick up a brand-name drug approval, the official process by which the FDA evaluates a new medication for safety and effectiveness before it can be sold in the U.S., you’re seeing the end result of years of testing, paperwork, and regulatory scrutiny. This isn’t just a stamp of approval—it’s a complex system designed to catch dangerous side effects, ensure consistent quality, and prove that the drug actually works better than a placebo. Behind every pill on the shelf is a mountain of data, clinical trials, and regulatory reviews that most patients never see.
The FDA, the U.S. agency responsible for regulating drugs, medical devices, and food safety. doesn’t just approve drugs—it fights to keep unsafe ones off the market. For a brand-name drug, the company must submit a New Drug Application (NDA), which includes data from animal studies, Phase I-III clinical trials, manufacturing details, and proposed labeling. The FDA reviews every piece. If there’s a red flag—like heart rhythm issues, liver toxicity, or unclear dosing—the application gets rejected or sent back for more data. That’s why some drugs never launch, even after spending hundreds of millions.
But approval doesn’t end there. Once a brand-name drug is on the market, the FDA keeps watching. Post-market studies, adverse event reports, and manufacturing inspections continue. And then comes the real challenge: generic drug approval, the process where manufacturers prove their version is therapeutically identical to the brand-name drug.. Generic makers don’t need to repeat all the clinical trials. Instead, they file an Abbreviated New Drug Application (ANDA), showing their product has the same active ingredient, strength, dosage form, and bioavailability. But here’s the catch: even small differences in inactive ingredients—like fillers or coatings—can cause side effects in sensitive patients. That’s why some people react differently to generics, even when the FDA says they’re equivalent.
And it’s not just about science. The ANDA, the application form generic drug companies must submit to the FDA to get approval for a copycat version of a brand-name drug. process is full of traps. One common reason for delays? FDA deficiency letters, official notices from the FDA pointing out missing or flawed data in a generic drug application.. These letters can delay approval for months or even years. They often cite issues like inconsistent drug substance purity, unclear manufacturing controls, or incomplete stability data. It’s not about being lazy—it’s about precision. One tiny error in a batch record can mean the difference between a safe drug and a dangerous one.
What’s happening now? The FDA is trying to speed things up. More generic applications are being reviewed in parallel, and the agency is sharing more feedback early in the process. But the system is still slow, and not all drugs get approved at the same rate. Some get fast-tracked. Others sit in limbo. And while patients want cheaper options, the system is built to protect them—even if it takes longer.
Below, you’ll find real-world examples of how this system works—what goes wrong, what gets approved, and how patients are affected. From failed applications to unexpected side effects, these posts show the human side of drug approval. Whether you’re a patient wondering why your generic doesn’t work the same, a pharmacist dealing with substitution rules, or just someone trying to understand why some drugs take forever to reach the market, this collection gives you the facts—not the marketing.