
Topical Antibiotic Selection Guide
Find your best topical antibiotic option
Answer a few questions about your infection to get a tailored recommendation.
Your Recommendation
Answer the questions above to get a personalized recommendation for your skin infection.
Key Takeaways
- Bactroban Ointment 5g delivers a high‑dose 2% mupirocin for tough skin infections.
- Fusidic Acid Cream works best for Staphylococcus aureus that’s resistant to other antibiotics.
- Retapamulin offers a non‑antibiotic‑class option with low resistance risk.
- Neosporin and Bacitracin are over‑the‑counter (OTC) but lack the potency of prescription mupirocin.
- Choosing the right ointment depends on infection severity, bacterial strain, and prescription access.
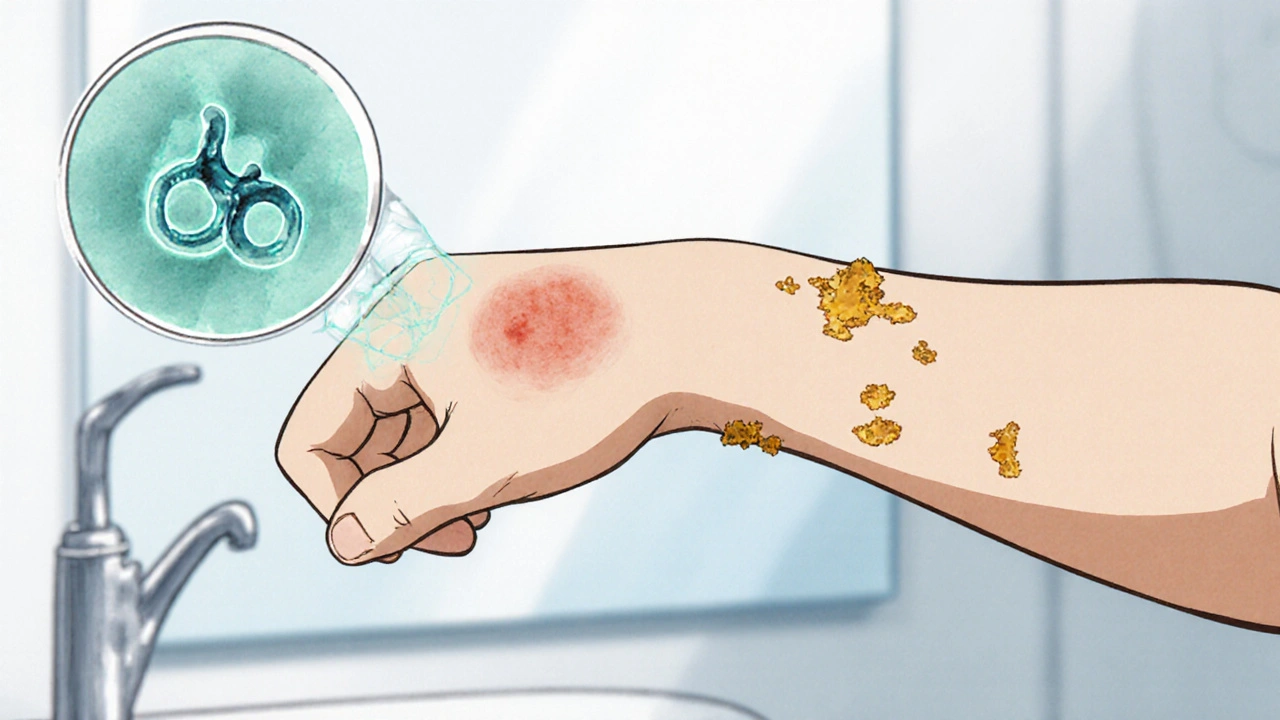
When treating skin infections, Bactroban Ointment 5g (Mupirocin) is a prescription‑only topical antibiotic containing 2% mupirocin, used to combat Staphylococcus aureus and Streptococcus pyogenes. But is it the best choice for every cut, scrape, or boil? This guide lines up Bactroban against the most common alternatives, breaks down how each works, and helps you pick the right cream or ointment for your situation.
What is Bactroban Ointment?
Bactroban is the brand name for mupirocin 2% ointment. It thins the outer skin layer, allowing the active ingredient to reach the bacteria that cause impetigo, infected eczema, and minor wounds. In the UK it’s a prescription‑only medicine (POM) and usually comes in a 5 g tube.
Key attributes:
- Active ingredient: mupirocin 2 % (20 mg/g)
- Formulation: ointment, easy to apply and stays on the skin for several hours
- Indications: impetigo, infected cuts, minor burns, and second‑line treatment for MRSA colonisation
How does mupirocin work?
Mupirocin stops bacteria from making essential proteins by inhibiting isoleucyl‑tRNA synthetase. Without this enzyme, bacterial cells can’t grow or reproduce. The result is rapid bacterial kill, especially against gram‑positive organisms like Staphylococcus aureus and Streptococcus pyogenes.
Because it targets a specific bacterial enzyme, resistance to mupirocin is slower to develop compared with broad‑spectrum antibiotics.
When should you use Bactroban?
Use Bactroban when a doctor confirms a bacterial skin infection that needs a potent topical agent. Typical scenarios include:
- Impetigo with honey‑coloured crusts
- Exposed eczema that’s become infected
- Post‑surgical wound infections where oral antibiotics are unsuitable
- MRSA decolonisation (off‑label, under specialist guidance)
It’s not meant for fungal infections, viral warts, or deep tissue abscesses that require systemic therapy.
Common Alternatives to Bactroban
Below are the top‑offered topical agents that doctors or pharmacists often suggest when Bactroban isn’t available, or when a different bacterial profile is suspected.
- Fusidic Acid Cream - a steroid‑compatible antibiotic effective against many Staphylococcus strains, especially when resistance to mupirocin is a concern.
- Retapamulin - a newer pleuromutilin class ointment (1 %) approved for uncomplicated skin infections; low cross‑resistance with other antibiotics.
- Clindamycin Gel - used for acne and occasionally for bacterial skin infections; works by blocking bacterial protein synthesis.
- Neosporin (triple‑antibiotic ointment) - contains bacitracin, neomycin, and polymyxin B; OTC, suitable for minor cuts but weaker against resistant Staph.
- Bacitracin ointment - single‑agent OTC, good for low‑risk superficial infections.
- Generic mupirocin (same active ingredient, often cheaper) - identical efficacy if sourced from a reputable pharmacy.
- Dicloxacillin Cream - a penicillin‑derived topical used in Europe for mild Staph infections.
Side‑by‑Side Comparison
| Attribute | Bactroban (Mupirocin 2%) | Fusidic Acid Cream | Retapamulin 1% | Neosporin (OTC) |
|---|---|---|---|---|
| Prescription status | Prescription‑only (POM) | Prescription‑only | Prescription‑only | Over‑the‑counter |
| Primary target | Gram‑positive (Staph, Strep) | Staphylococcus aureus (incl. MRSA‑low) | Gram‑positive skin pathogens | Minor superficial bacteria |
| Resistance risk | Low (but reported in high‑dose use) | Moderate (fusidic acid resistance rising) | Very low (new class) | Higher (multiple agents, OTC misuse) |
| Formulation | Ointment (5 g tube) | Cream (15 g tube) | Ointment (5 g tube) | Ointment (5 g tube) |
| Typical cost (UK) | £15‑£20 | £12‑£18 | £30‑£35 | £5‑£7 |
| Common side effects | Mild irritation, itching | Burning, redness | Transient itching | Allergic dermatitis (neomycin) |
Pros and Cons of Each Option
Bactroban - Pros: high potency, proven against MRSA colonisation, once‑daily application works for most infections. Cons: prescription needed, slightly pricey, may cause local irritation.
Fusidic Acid - Pros: excellent for penicillin‑allergic patients, good stability in cream form. Cons: growing resistance, less effective for deep impetigo.
Retapamulin - Pros: new mechanism, low cross‑resistance, suitable for patients with multiple antibiotic failures. Cons: highest cost, limited to uncomplicated infections.
Neosporin - Pros: easy to buy, cheap, covers a range of bacteria. Cons: weak against resistant Staph, contains neomycin (allergy risk).

How to Choose the Right Topical Antibiotic
- Identify the bacterial culprit. If a culture shows MRSA, Bactroban or Retapamulin are preferred.
- Check prescription access. For OTC‑only shoppers, Neosporin or Bacitracin may be the only option.
- Consider resistance trends. In areas where fusidic acid resistance exceeds 20 %, avoid that cream.
- Assess cost and convenience. Generic mupirocin offers the same effect at a lower price if insurance covers it.
- Account for allergies. Patients allergic to neomycin should skip Neosporin; those with penicillin allergy may prefer fusidic acid.
Always discuss with a pharmacist or GP before switching, especially for chronic skin conditions.
Frequently Asked Questions
Can I use Bactroban for fungal infections?
No. Bactroban targets bacteria only. For fungal skin infections you need an antifungal such as clotrimazole or terbinafine.
How long should I apply Bactroban?
Typical courses last 5‑7 days, applied twice daily. Always follow your prescriber’s instructions.
Is generic mupirocin as effective as Bactroban?
Yes, if the generic product contains the same 2 % mupirocin and is sourced from a reputable pharmacy.
Can I use fusidic acid cream on a child?
It’s safe for children over 2 years, but you need a prescription. Always check dosage and duration with a paediatrician.
Why does Bactroban sometimes cause itching?
The ointment base can be greasy, and the active ingredient may irritate sensitive skin. If itching is severe, stop use and consult a pharmacist.
Bottom Line
If you need a strong, proven antibiotic for impetigo or MRSA‑related skin issues, Bactroban Ointment 5 g (mupirocin) remains the go‑to choice-provided you can get a prescription. For milder infections, or when cost is a barrier, fusidic acid cream, retapamulin, or OTC options like Neosporin can fill the gap, but each comes with its own trade‑offs.
Next steps? Talk to your GP or community pharmacist, get a culture if the infection is persistent, and pick the product that matches the bacteria, your budget, and any allergy concerns.

Kala Rani
October 25, 2025 AT 19:28I get why Bactroban’s hype is strong yet the same bacteria often bow to a simple OTC tube of Neosporin
Octavia Clahar
October 26, 2025 AT 13:00Hey everyone, love the thoroughness of this guide but let’s be honest – most of us never need a prescription when a tiny cut just calls for a dab of Bacitracin
Cheyanne Moxley
October 27, 2025 AT 07:36Honestly you’re missing the point using OTC creams on MRSA‑related impetigo is downright irresponsible and puts everyone at risk
Kevin Stratton
October 28, 2025 AT 02:13When we look at the landscape of topical antibiotics, Bactroban stands as a microcosm of modern medicine's promise and its perils. Its 2 % mupirocin concentration is engineered to breach the bacterial fortress and halt protein synthesis, a marvel of biochemical precision. Yet the very act of targeting a specific enzymatic pathway invites a subtle dance between efficacy and the slow rise of resistance. Patients often assume that a prescription automatically guarantees safety, forgetting that skin is a complex ecosystem teeming with commensals. Disrupting that balance with a potent agent can, in rare cases, pave the way for opportunistic colonizers to take hold. From an ethical standpoint, prescribing Bactroban without confirming a bacterial culture may be an overreach, especially when cheaper generic mupirocin exists. Economic considerations also loom large; a £15 course can be a burden for those without insurance, nudging them toward suboptimal OTC substitutes. On the other hand, for confirmed MRSA colonisation, the risk–benefit calculus tilts decisively toward the prescription ointment. Clinicians must therefore weigh microbial data, patient history, and socioeconomic factors before reaching for the tube. The table in the article neatly juxtaposes Bactroban with fusidic acid, retapamulin, and Neosporin, highlighting that potency is not the sole metric of suitability. For example, fusidic acid’s rising resistance rates in certain regions demand vigilant stewardship. Retapamulin, while promising a new mechanism, carries a price tag that can alienate many. OTC options like Neosporin serve a niche for superficial cuts but falter against resistant staphylococci. Thus, the decision tree is less about a single ‘best’ cream and more about aligning therapy with the infection’s microbiology. Patients should be encouraged to seek proper diagnosis and not self‑medicate with whatever is at hand. In the end, Bactroban remains a valuable tool, but like any tool, its impact depends on the hand that wields it 🙂.
Megan Dicochea
October 28, 2025 AT 20:50I appreciate the clear breakdown of cost – Bactroban at £15‑£20 can feel steep but the generic 2 % mupirocin can shave that down dramatically
Jennie Smith
October 29, 2025 AT 15:26Your point hits the sweet spot – think of the generic as the hidden gem that shines when you dig a little deeper into the pharmacy aisle
Anurag Ranjan
October 30, 2025 AT 10:03For anyone debating Bactroban versus fusidic, remember that fusidic acid resistance is climbing above 20 % in many regions, so culture results guide the choice
James Doyle
October 31, 2025 AT 04:40From a pharmacodynamic perspective, Bactroban’s bactericidal activity stems from its inhibition of isoleucyl‑tRNA synthetase, a mechanism that confers a low propensity for resistance development relative to beta‑lactam agents; however, the clinical utility cannot be divorced from real‑world adherence considerations. Moreover, the ointment base ensures prolonged skin contact, which enhances drug absorption but may also increase local irritation in sensitive patients. The cost factor cannot be ignored either, as the prescription price often limits accessibility for low‑income individuals, pushing them toward suboptimal OTC alternatives. In practice, physicians should balance the drug’s potency against patient compliance, potential side effects, and the local resistance patterns before committing to a Bactroban regimen.
Edward Brown
October 31, 2025 AT 23:16While you wax poetic about enzymatic inhibition don’t forget the pharma lobby pushes Bactroban to keep cheaper OTC alternatives out of the market ensuring a steady stream of prescription revenue
Suzanne Carawan
November 1, 2025 AT 17:53Oh sure because everyone loves waiting weeks for a prescription
eko lennon
November 2, 2025 AT 12:30The saga of choosing a skin ointment feels like a Shakespearean tragedy unfolding on the bathroom counter. You stand there, tube in hand, contemplating the fate of a tiny cut that could either heal gracefully or become a battlefield of resistant microbes. Bactroban looms like a noble knight, armored with 2 % mupirocin, promising swift victory over staphylococcal foes. Yet the price tag reads like a royal ransom, and the prescription requirement feels like a gatekeeper demanding tribute. Meanwhile, the humble Neosporin whispers sweet nothings, cheap and readily available, but its promises crumble when faced with a stubborn MRSA. The drama intensifies as you weigh the risk of resistance against the allure of convenience, each option starring its own chorus of side effects and anecdotes from fellow sufferers. In the end, the decision becomes a personal epic, a testament to how even the simplest medical choices can echo with the weight of destiny.
Sunita Basnet
November 3, 2025 AT 07:06What a vivid tale! Remember, sometimes the “knight” isn’t the only hero – a modest OTC cream can still save the day if the infection is mild, so keep your options flexible and your spirit optimistic.
Melody Barton
November 4, 2025 AT 01:43Listen up – if you’re dealing with a legit infection don’t waste time debating, get the prescription Bactroban and apply it correctly, or you’ll just be setting yourself up for a nasty flare‑up.
Justin Scherer
November 4, 2025 AT 20:20I hear you the direct approach works but it’s worth double‑checking with a pharmacist to avoid allergic reactions and make sure the dosage is right.
Pamela Clark
November 5, 2025 AT 14:56Oh brilliant, another layperson review of top‑tier dermatology – because who needs actual clinical training when you have the internet, right?